Articles
- Page Path
- HOME > Epidemiol Health > Volume 45; 2023 > Article
-
Original Article
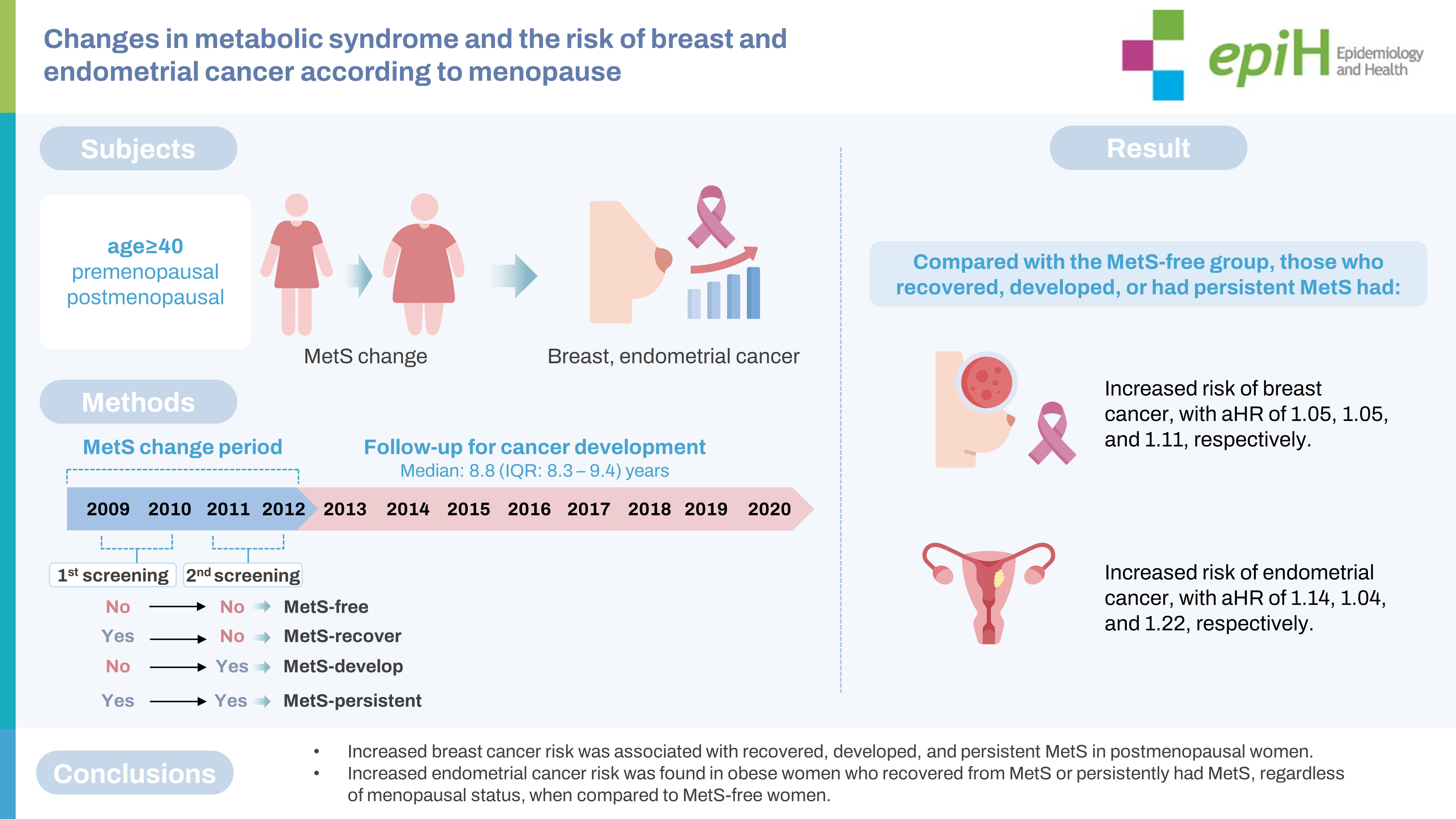
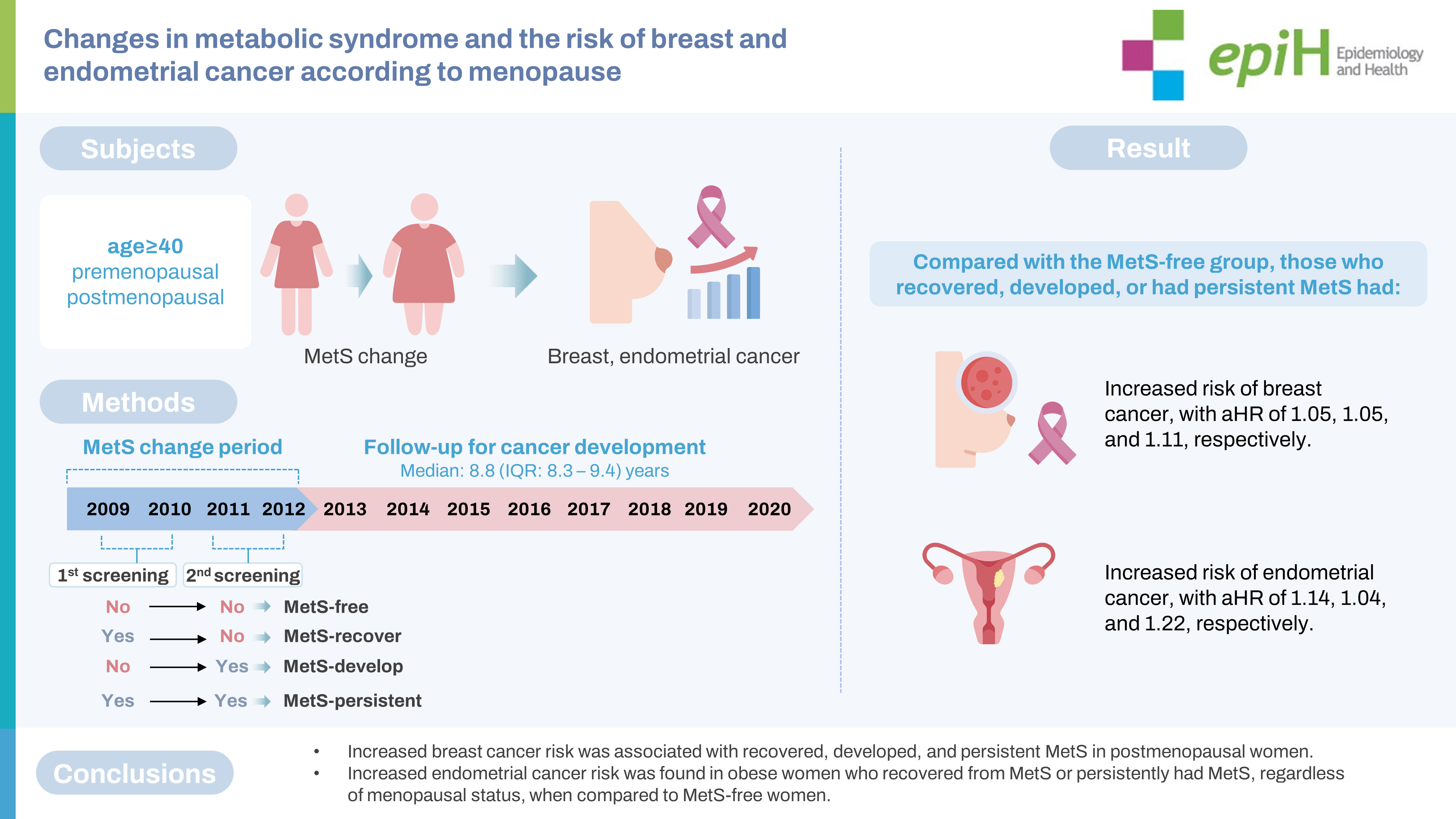
Changes in metabolic syndrome and the risk of breast and endometrial cancer according to menopause in Korean women -
Thi Xuan Mai Tran1,2
 , Soyeoun Kim1,2
, Soyeoun Kim1,2 , Boyoung Park1,3
, Boyoung Park1,3
-
Epidemiol Health 2023;45:e2023049.
DOI: https://doi.org/10.4178/epih.e2023049
Published online: May 1, 2023
1Department of Preventive Medicine, Hanyang University College of Medicine, Seoul, Korea
2Institute for Health and Society, Hanyang University, Seoul, Korea
3Hanyang Institute of Bioscience and Biotechnology, Hanyang University, Seoul, Korea
- Correspondence: Boyoung Park Department of Preventive Medicine, Hanyang University College of Medicine, 222 Wangsimni-ro, Seongdong-gu, Seoul 04763, Korea E-mail: hayejine@hanyang.ac.kr
© 2023, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
- This study investigated how changes in metabolic syndrome (MetS) are associated with the subsequent risk of breast and endometrial cancer according to menopausal status.
-
METHODS
- This cohort study, using data from the National Health Insurance Service database, included women aged ≥40 years who underwent 2 biennial cancer screenings (2009-2010 and 2011-2012) and were followed up until 2020. Participants were grouped into MetS-free, MetS-recovery, MetS-development, and MetS-persistent groups. Menopausal status (premenopausal, perimenopausal, and postmenopausal) was assessed at 2 screenings. Cox proportional hazard regression was used to assess the association between MetS changes and cancer risk.
-
RESULTS
- In 3,031,980 women, breast and endometrial cancers were detected in 39,184 and 4,298, respectively. Compared with the MetS-free group, those who recovered, developed, or had persistent MetS showed an increased risk of breast cancer, with adjusted hazard ratios (aHRs) of 1.05, 1.05, and 1.11, respectively (p<0.005). MetS persistence was associated with an increased risk of breast cancer in postmenopausal women (aHR, 1.12, 95% confidence interval [CI], 1.08 to 1.16) but not in premenopausal or perimenopausal women. MetS persistence was associated with an increased risk of endometrial cancer in premenopausal, perimenopausal, and postmenopausal women, with aHRs of 1.41 (95% CI, 1.17 to 1.70), 1.59 (95% CI, 1.19 to 2.12), and 1.47 (95% CI, 1.32 to 1.63), respectively.
-
CONCLUSIONS
- Increased breast cancer risk was associated with recovered, developed, and persistent MetS in postmenopausal women. Meanwhile, increased endometrial cancer risk was found in obese women who recovered from MetS or persistently had MetS, regardless of menopausal status, when compared to MetS-free women.
- Metabolic syndrome (MetS) is a growing global problem [1,2]. MetS comprises a cluster of risk factors, including central adiposity, impaired fasting plasma glucose (FPG), elevated blood pressure (BP), elevated triglyceride (TG) levels, and low high-density lipoprotein (HDL) cholesterol levels. Breast cancer is the most commonly diagnosed cancer worldwide, accounting for 11.7% of all new cancer cases in 2020 [3]. In Korea, the burden of breast cancer has gradually increased over the last decade [4,5]. While endometrial cancer is less common, its incidence also has increased steadily in Korea [6]. Despite a generally decreasing trend in the incidence of total cancer and most cancer types, breast and endometrial cancer have shown steadily increasing trends in Korea since 1999, when the first national cancer statistics were published [7]. MetS has been reported to be associated with an increased risk of various malignancies, including endometrial cancer [8,9] and breast cancer [10,11]. The biological mechanisms underlying the association between MetS and breast and endometrial cancer might reflect the role of MetS as a potential surrogate marker for obesity, an unhealthy diet, and the aging process [1,12].
- Previous studies have found an increased risk of breast cancer in postmenopausal, but not premenopausal women with MetS, suggesting that the association between MetS and breast cancer might differ depending on menopausal status [11-13], although evidence in perimenopausal women has remained limited. In addition, the association between adiposity and risk of breast cancer has shown opposite directions in premenopausal and postmenopausal women; high body mass index (BMI) had no association or was associated with a reduced risk of breast cancer in premenopausal women [14], whereas increased adiposity was positively associated with an increased risk of breast cancer in postmenopausal women [15]. Thus, the relationship between MetS and the risk of breast cancer might vary according to menopausal status and should be considered together with BMI status. While an association between MetS and breast cancer was found only in postmenopausal women [11-13], an increased risk of endometrial cancer associated with MetS was found in both premenopausal and postmenopausal women [8,9,16], with an even higher risk in premenopausal women [16].
- Despite the existence of comprehensive evidence suggesting the important role of MetS as a risk factor for breast and endometrial cancer in postmenopausal women, it is unclear how changes in MetS affect the risk of cancer. Thus, this study aimed to assess the associations between longitudinal changes in MetS and the risk of developing breast and endometrial cancer. Because menopause has been proposed as an important factor contributing to an increased prevalence of MetS [17], we assessed the associations between changes in MetS and cancer development separately for premenopausal, perimenopausal, and postmenopausal women.
INTRODUCTION
- Study sample or population
- This study used customized data from the National Health Insurance Service (NHIS) database [18]. In Korea, the NHIS provides biennial health-screening examinations for all Koreans to assess the risk of chronic diseases. All inpatient and outpatient visits, procedures, and prescriptions are recorded in the database. The initial study database included women aged ≥ 40 years who underwent national breast cancer screening between 2009 and 2010 (n= 5,105,129) and between 2011 and 2012 (n= 5,641,764). Only participants who underwent screening during both periods were initially considered (n=3,299,776) (Figure 1). After excluding those who were diagnosed with cancer before the second screening or within 6 months after the second screening and those with missing information on MetS or missing menopausal status, the final dataset included 3,031,980 women.
- Measures of changes in metabolic syndrome
- MetS was defined based on the modified National Cholesterol Rationale Education Program Adult Treatment Program (NECP-ATP III) [19], comprising the following 5 components: waist circumference (WC) ≥ 80 cm, FPG ≥ 100 mg/dL, TG level ≥ 150 mg/dL, HDL level < 50 mg/dL, and elevated BP (systolic ≥ 130 mmHg or diastolic ≥ 85 mmHg). The presence of each component of MetS was counted and added to obtain a score for each subject. An individual was defined as having MetS if he or she had 3 or more of the 5 above-mentioned components.
- According to changes in MetS status between the first screening in 2009-2010 and the second screening in 2011-2012, participants were grouped into the following categories: MetS-free (no MetS at both screenings), MetS-recovered (MetS at the first screening and no MetS at the second screening), MetS-developed (no MetS at the first screening and MetS at the second screening), and MetS-persistent (MetS at both screenings) (Figure 2).
- In addition, changes in each component of MetS status between the first and second screenings were analyzed according to each menopausal group. Changes in MetS scores and the presence of each component of MetS between the first and second measurements and their associations with breast and endometrial cancer were assessed as described above.
- Measures of outcomes
- The main outcomes were incident breast cancer and endometrial cancer, which were ascertained from the healthcare utilization database of the NHID. In Korea, patients with cancer have a special co-payment reduction program called the rare incurable disease system, and cancer cases are registered in this system from the time of diagnosis. In this study, the incidence of cancer events was defined as cases having both the corresponding International Classification of Diseases code (C50 or D05 for breast cancer and C54 for endometrial cancer) and a rare incurable disease system code [20]. This approach is sufficiently reliable and has been used in previous studies [21]. Cancer case tracking was conducted until December 2020. If a woman developed both breast cancer and endometrial cancer, the first cancer was considered an outcome.
- Measures of other covariates
- Menopausal status was measured at both screenings using the question: “What is your current menopausal status?” with the following response options: still menstruating, have had a hysterectomy, and have undergone menopause. Women who reported having undergone menopause were further asked to report the age at which they underwent menopause. Based on this information, menopausal status was classified into the following categories: premenopausal, perimenopausal, and postmenopausal. Perimenopausal women included those whose status changed from premenopausal to postmenopausal between the 2 screenings.
- Other risk factors measured during the second screening were considered covariates in our analysis. Height and weight were measured on the date of screening and used to calculate the BMI. According to the Asia-Pacific classification, BMI was categorized into the following groups [22]: underweight (BMI < 18.5 kg/m2), normal (18.5 to < 23.0 kg/m2), overweight (23.0 to < 25.0 kg/m2), and obese (≥ 25.0 kg/m2).
- All participants in the national health screening were asked to complete a self-report questionnaire to assess their health behaviors and conditions before the screening. We included the following variables as covariates in our analysis: age at screening, age at menarche (< 15, 15-16, and ≥ 17 years, and missing), child delivery (0, 1, ≥ 2, and missing), duration of breastfeeding (never, < 1 and ≥ 1 year, and missing), oral contraceptive use (never, ever, and missing), family history of breast cancer in first-degree relatives (yes and no), vigorous or moderate physical activity per week (once or more per week, none, or missing), smoking status (never, ever, or missing), alcohol consumption (none, once and ≥ 2 times per week, and missing), and breast density (4 levels). For perimenopausal and postmenopausal women, we further adjusted for age at menopause (< 45, 45-52, and ≥ 53 years, and missing) and hormone replacement therapy for postmenopausal women (never, < 5 and ≥ 5 years, and missing). Only age at screening was expressed as a continuous variable, and the rest of the variables were expressed as categorical variables.
- Statistical analysis
- Descriptive statistics of the baseline characteristics of the participants, MetS status at the first and second screenings, and changes in MetS according to menopausal status are presented. To quantify the association between changes in MetS and cancer development, we performed Cox proportional hazards regression analysis to estimate hazard ratios (HRs) and 95% confidence intervals (CIs). The time-to-event period was counted in days from the date of the second screening to the date of the event (breast or endometrial cancer diagnosis), the development of other types of cancer, death, or the end of the study period. The risk of cancer was calculated with adjustment for other covariates. Missing covariate values were treated as dummy variables (separate categories).
- We assessed the risk of cancer in the different MetS-change groups compared to the MetS-free group. The MetS-change variable, with 4 values corresponding to the four MetS-change groups, was included in a regression model, and the MetS-free group was used as the reference. We assessed the risk of cancer in the total population and each menopausal group. Three models were used in this study. The first was adjusted for age at the time of screening. The second and third covariates were additionally adjusted for other covariates, with and without adjustment for BMI. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
- Ethics statement
- This study was approved by the Institutional Review Board of Hanyang University College of Medicine (approval No. HYUIRB-202106-003-1). The NHIS database approved the use of the National Health Insurance Service-National Health Information Database (NHIS-NHID). In this study, all members of the screened population agreed to transfer their screening results to the NHIS-NHID. The NHIS database was constructed for individual identification after anonymization.
MATERIALS AND METHODS
- Characteristics of the study population
- At the time of screening, the mean± standard deviation (SD) age of 3,031,980 women was 55.5 ± 10.1 years. Among them, 788,926 (26.0%), 229,951 (7.6%), and 2,013,103 (66.4%) women were in the premenopausal, perimenopausal, and postmenopausal phases, respectively (Table 1). The proportions of overweight and obese women in the total population were 25.7% and 33.6%, respectively. After a median follow-up of 8.8 years (interquartile range [IQR], 8.3 to 9.4), 39,148 breast cancer cases and 4,298 endometrial cancer cases were detected.
- At the first screening, the proportion of women with MetS (≥ 3 criteria) was 26.1% in the total population and was higher in postmenopausal women (32.9%) than in perimenopausal or premenopausal women (17.5 and 11.4%, respectively) (Supplementary Material 1). Between the 2 screenings, 62.7% of women were MetS-free, 10.8% recovered from MetS, 11.1% developed MetS, and 15.4% had persistent MetS. The highest percentage of MetS persistence was found among postmenopausal women (19.8%), followed by perimenopausal (9.5%) and premenopausal women (5.7%). Characteristics according to changes in MetS are described in Table 2. Women with persistent MetS had the highest mean± SD age at 61.3± 9.2 years, and women who were MetS-free had the lowest mean± SD age at 53.4± 10.0 years.
- Association between changes in metabolic syndrome and the risk of breast cancer
- In postmenopausal women, those in the MetS-recovered, MetS-developed, or MetS-persistent groups had a higher risk of breast cancer than those in the MetS-free group, with adjusted HRs of 1.19 (95% CI, 1.14 to 1.25), 1.19 (95% CI, 1.14 to 1.24), and 1.33 (95% CI, 1.28 to 1.38), respectively (Table 3). After additionally adjusting for BMI, the HR decreased (1.09, 1.06, and 1.12, respectively), but remained statistically significant. No significant association was found between changes in MetS and the risk of breast cancer after adjusting for BMI in premenopausal and perimenopausal women. Consistent findings was observed in subgroup according to age group (Supplementary Material 2). A subgroup analysis revealed that both non-obese and obese women had an increased risk of postmenopausal breast cancer associated with changes in MetS (Supplementary Material 3).
- Association between changes in metabolic syndrome and risk of endometrial cancer
- Changes in MetS were also associated with the risk for endometrial cancer (Table 4). Before adjusting for BMI, women in the MetS-recovered, MetS-developed, and MetS-persistent groups had a 1.36-fold (95% CI, 1.23 to 1.50), 1.28-fold (95% CI, 1.16 to 1.41), and 1.65-fold (95% CI, 1.51 to 1.79) increased risk of endometrial cancer compared to MetS-free women. After adjusting for BMI, the strength of the association decreased, but remained statistically significant, with adjusted HRs of 1.14, 1.04, and 1.22, respectively. Persistent MetS was associated with an increased risk of endometrial cancer in premenopausal and perimenopausal women, with adjusted HRs of 1.41 (95% CI, 1.17 to 1.70) and 1.59 (95% CI, 1.19 to 2.12). Postmenopausal women in the MetS-recovered, MetS-developed, and MetS-persistent groups had a higher risk of endometrial cancer than the MetS-free group, with adjusted HRs of 1.24 (95% CI, 1.09 to 1.40), 1.14 (95% CI, 1.00 to 1.30), and 1.47 (95% CI, 1.32 to 1.63). When stratified by obesity status at the second screening, in non-obese women, a significantly elevated risk of endometrial cancer was found only in postmenopausal women in the MetS-developed and MetS-persistent groups compared with the MetS-free group, with HRs of 1.22 (95% CI 1.02 to 1.45) and 1.34 (95% CI 1.12 to 1.60), respectively (Table 5). Meanwhile, obesity in the MetS-persistent group was associated with an elevated risk of endometrial cancer in premenopausal, perimenopausal, and postmenopausal women (adjusted HRs of 1.49, 1.76, and 1.46, respectively).
RESULTS
MetS and its change between the 2 screenings
- This study reports an elevated risk of breast cancer in postmenopausal women who recovered from MetS, developed MetS, and had persistent MetS compared to women who remained free of MetS, after adjusting for BMI and other covariates, but not in premenopausal or perimenopausal women. The risk of endometrial cancer was found to be higher in MetS-persistent and MetS-recovered premenopausal and postmenopausal women. An increased risk of endometrial cancer was also observed in perimenopausal women with MetS-persistent status. When stratifying by obesity status, consistent results were observed in obese women. In non-obese women, an increased endometrial cancer risk associated with MetS development and persistence was only observed in postmenopausal women.
- The increased risk of breast cancer in postmenopausal women with MetS is similar to that reported in previous studies [13,23]. A pooled analysis from 3 previous cohort studies reported no significant relationship between MetS and the risk of breast cancer in premenopausal women (risk ratio [RR], 0.91; 95% CI, 0.64 to 1.29) and a 2-fold increased risk in postmenopausal women (RR, 2.01; 95% CI, 1.55 to 2.60) [13]. Regarding the association with changes in MetS, a previous study in Korean women [24] also found an increased risk of breast cancer in women who recovered from MetS, developed MetS, or had persistent MetS. However, a limitation of the previous study [24] was the short follow-up period for cancer development, which was improved in our study (8.6 vs. 6.4 years). In addition, a previous study [24] did not adjust for other important factors of breast cancer, such as reproductive factors, and did not consider the impact of BMI in the analysis. While BMI is an indicator of general obesity, central obesity is an important component of MetS. Although general obesity (assessed by BMI) and MetS are closely related to each other [25], general obesity and the presence of MetS do not always co-occur, suggesting the possibility of an independent role for general obesity and MetS in health status. To date, only a few studies have examined the relative contributions of general obesity, central obesity (assessed by WC), and MetS to the risk of breast cancer [26-28]. Our findings are consistent with the results of the Sister Study [28], which found that postmenopausal women who were metabolically unhealthy, including recovered, developed, and persistent groups, had an elevated risk of breast cancer regardless of their BMI. In this study, postmenopausal women whose MetS status had changed were at an increased risk of breast cancer with similar HRs (1.09 and 1.06 for the MetS-recovered and developed groups, respectively). Based on these results, the effect of short-term changes in MetS on the risk of breast cancer is minimal. Considering the higher HR of the MetS-persistent group compared with other MetS statuses, long-term exposure to the unhealthy status of MetS would affect the future risk of breast cancer in postmenopausal women. More longitudinal studies are needed to determine the duration of MetS, its phenotype, and the future risk of breast cancer.
- The association between MetS and the risk of endometrial cancer has been well documented [8,29]. An interesting finding of this study is that the association between changes in MetS and the risk of endometrial cancer differed according to general obesity and menopausal status. Associations between MetS recovery, MetS persistence, and the risk of endometrial cancer were observed in obese women, irrespective of menopausal status. Several studies have found an association between MetS and an increased risk of endometrial cancer in obese women [12,30,31]. Even though we did not know participants’ MetS status before the first screening, the total exposure duration of MetS in MetS-recovered obese women was expected to be longer than that in women with newly developed MetS. To confirm this hypothesis, prospective studies on the development of MetS and endometrial cancer in young women need to be conducted. In this study, the association between endometrial cancer and MetS persistence was observed only in postmenopausal, non-obese women. The increased risk of endometrial cancer in non-obese women who developed MetS between the first and second screening could be due to weight gain within the normal range (Supplementary Material 4), followed by worsening metabolic health. This might suggest a population subgroup that is susceptible to disease risk with an increased weight even within the normal range, followed by MetS development and further risk of endometrial cancer. Non-obese women with metabolic abnormalities showed lower circulating insulin levels than obese women [32]. Despite the general non-association between MetS and endometrial cancer in non-obese women [12,30,31], postmenopausal women who developed MetS or had persistent MetS were at a higher risk of endometrial cancer than premenopausal or perimenopausal women. The increased disease risk in postmenopausal women with MetS compared to women without MetS, including cancer, cardiovascular diseases, and other chronic diseases, has been well identified. However, few studies have explored this issue in premenopausal women. Considering the very low incidence of endometrial cancer in young women [33] and the increased incidence of endometrial cancer with increasing age [34,35], non-obese premenopausal and perimenopausal women would have too low a risk of developing endometrial cancer during the follow-up period to obtain meaningful results.
- Shared etiologies and risk factors between breast cancer and endometrial cancer have been identified [36,37], as have shared physiological mechanisms underlying the association of MetS with breast and endometrial cancer [9,38,39]. Obesity-related insulin resistance, hyperinsulinemia, impaired glucose tolerance, dyslipidemia, and visceral obesity are some of the biological mechanisms that contribute to the impact of MetS on the risk of endometrial cancer [9,39]. Obesity-related metabolic factors, including serum TG levels, were shown to be associated with increased endometrial cancer risk [40]; however, further adjustment for BMI tended to attenuate the association, which was likewise observed in our results (Supplementary Material 5). Insulin resistance, inflammation, and estrogen from adipose tissue have been suggested to be the main physiological mechanisms involved in the increased risk of breast cancer related to MetS in postmenopausal women [38]. The different associations between changes in MetS and breast and endometrial cancer based on menopausal status and obesity may reflect the different age-specific incidence rates of those cancers [33,41].
- This study has several limitations. First, the median follow-up time was less than 9 years, which was relatively short and might be insufficient to assess the effect of MetS on the risk of cancer, as a relatively slowly developing disease. Second, our database may have been subjected to selection bias because women who regularly undergo cancer screening may be a particularly health-conscious segment of the population. Third, data on MetS status before the first screening were not available and were therefore not considered in the current findings. This left-truncated feature of the database might explain some of the higher HRs observed in women who recovered from MetS relative to those observed in the MetS-free group. Finally, this study assessed changes in MetS using only 2 biennial cancer screenings. The short period between the 2 measurements and the limited number of MetS assessments (only 2 measurements) may not have fully captured the trajectory of MetS changes over time. As MetS is a chronic condition that can develop over many years, there may have been some misclassification of participants’ MetS statuses between the 2 screenings owing to transient changes in the MetS criteria. This misclassification of MetS status may have led to an underestimation or overestimation of the impact of MetS changes on cancer risk. Thus, future studies with different approaches for assessing MetS changes—either with longer gaps between 2 assessments or more total MetS assessments—may be helpful for overcoming our study’s limitations.
- While increased breast and endometrial cancer risks associated with MetS have been previously reported [9,13], those studies used only single measurements of MetS. In this study, our results were based on changes in MetS. Our findings suggest that alterations in MetS status and sustained MetS, especially in postmenopausal women, are associated with increased risks of breast and endometrial cancer. Thus, these results imply that improvements in MetS status may help to reduce the risk of developing these cancers. Transitions in MetS status may be achieved through lifestyle modifications such as smoking cessation, increased physical activity, diet, and maintaining a healthy weight.
- Despite these limitations, our study has several strengths. First, this study included a very large, women, population-based database with a longitudinal assessment of MetS status and an accurate assessment of cancer cases. In addition, a wide range of well-established confounding factors associated with breast cancer and endometrial cancer were adjusted for, such as reproductive factors and family history of cancer. We also excluded prevalent cancer cases that developed within 6 months of the last assessment of MetS to avoid the potential inverse causality between changes in MetS and cancer development.
- In conclusion, this cohort study found that changes in MetS were associated with an increased risk of breast and endometrial cancer in Korean women aged ≥ 40 years, with the highest risk in those who had persistent MetS. MetS-persistent status in postmenopausal women was associated with increased breast cancer risk. A higher risk of endometrial cancer was found in obese women who recovered from MetS or had persistent MetS, whereas in non-obese women, MetS only showed significant associations in the postmenopausal subgroup. Our findings add more evidence to support the idea that not only MetS itself, but also its changes, are important etiologic factors for breast and endometrial cancer. Hence, nutritional and lifestyle modifications to alleviate MetS may help reduce the risk of these cancers.
DISCUSSION
- The data that support the findings of this study are available on the website of the National Health Insurance Sharing Service (https://nhiss.nhis.or.kr/). We accessed the database after submitting the study protocol, the IRB approval document, and the reviewed request form by the committee. Further information is available from the corresponding author upon request.
DATA AVAILABILITY
SUPPLEMENTARY MATERIALS
Supplementary Material 1.
Supplementary Material 2
Supplementary Material 3
Supplementary Material 4
Supplementary Material 5
-
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare for this study.
-
FUNDING
This research was supported by the National Research Foundation of Korea grant funded by the Korean government (MSIT) (grant No. 2021R1A2C1011958) and the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (grant No. RS-2023-00241942). This work was partly supported by Institute of Information & communications Technology Planning & Evaluation (IITP) grant funded by the Korea government (MSIT) (grant No. 2020-0-01373, Artificial Intelligence Graduate School Program [Hanyang University]) and the research fund of Hanyang University (HY-202300000000174).
-
AUTHOR CONTRIBUTIONS
Conceptualization: Tran TXM, Park B. Data curation: Kim S. Formal analysis: Tran TXM. Funding acquisition: Park B. Methodology: Tran TXM. Project administration: Kim S. Visualization: Tran TXM. Writing – original draft: Tran TXM. Writing – review & editing: Tran TXM, Kim S, Park B.
NOTES
ACKNOWLEDGEMENTS
| Changes in MetS | No. of cases | Person-years | Model 11 | Model 22 | Model 33 | |
|---|---|---|---|---|---|---|
| Total | ||||||
| Free | 25,919 | 16,428,716 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 3,772 | 2,804,089 | 1.05 (1.02, 1.09) | 1.13 (1.10, 1.18) | 1.05 (1.02, 1.09) | |
| Developed | 4,046 | 2,897,548 | 1.07 (1.03, 1.10) | 1.15 (1.11, 1.19) | 1.05 (1.02, 1.09) | |
| Persistent | 5,411 | 3,964,028 | 1.14 (1.11, 1.18) | 1.26 (1.22, 1.30) | 1.11 (1.00, 1.14) | |
| Premenopausal | ||||||
| Free | 12,167 | 5,594,895 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 771 | 384,776 | 0.93 (0.87, 1.00) | 1.00 (0.93, 1.08) | 0.97 (0.90, 1.04) | |
| Developed | 983 | 449,817 | 1.02 (0.95, 1.09) | 1.09 (1.02, 1.16) | 1.05 (0.98, 1.12) | |
| Persistent | 817 | 386,732 | 0.99 (0.92, 1.06) | 1.09 (1.01, 1.17) | 1.03 (0.95, 1.11) | |
| Perimenopausal | ||||||
| Free | 2,399 | 1,450,028 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 286 | 159,890 | 1.10 (0.97, 1.24) | 1.18 (1.04, 1.33) | 1.12 (0.99, 1.27) | |
| Developed | 331 | 191,356 | 1.06 (0.94, 1.19) | 1.14 (1.02, 1.28) | 1.07 (0.95, 1.21) | |
| Persistent | 341 | 187,006 | 1.12 (1.00, 1.26) | 1.25 (1.11, 1.40) | 1.13 (1.00, 1.28) | |
| Postmenopausal | ||||||
| Free | 11,353 | 9,383,793 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 2,715 | 2,259,422 | 1.11 (1.07, 1.16) | 1.19 (1.14, 1.25) | 1.09 (1.04, 1.14) | |
| Developed | 2,732 | 2,256,375 | 1.10 (1.06, 1.15) | 1.19 (1.14, 1.24) | 1.06 (1.02, 1.11) | |
| Persistent | 4,253 | 3,390,290 | 1.21 (1.16, 1.25) | 1.33 (1.28, 1.38) | 1.12 (1.08, 1.16) | |
Values are presented as hazard ratio (95% confidence interval).
1 Model 1 was adjusted for age at screening.
2 Model 2 was adjusted for age at screening, age at menarche, child delivery, breastfeeding, oral contraceptive use, family history of breast cancer, vigorous or moderate physical activity, smoking status, alcohol consumption, and breast density; For perimenopausal and postmenopausal women, the model was additionally adjusted for age at menopause and the use of hormone replacement therapy.
3 Model 3 was adjusted for covariates similar to model 2, with the addition of body mass index.
| Changes in MetS | No. of cases | Person-years | Model 11 | Model 22 | Model 33 | |
|---|---|---|---|---|---|---|
| Total | ||||||
| Free | 2,568 | 16,428,716 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 482 | 2,804,089 | 1.33 (1.20, 1.46) | 1.36 (1.23, 1.50) | 1.14 (1.03, 1.27) | |
| Developed | 480 | 2,897,548 | 1.25 (1.13, 1.38) | 1.28 (1.16, 1.41) | 1.04 (0.94, 1.15) | |
| Persistent | 768 | 3,964,028 | 1.58 (1.45, 1.72) | 1.65 (1.51, 1.79) | 1.22 (1.11, 1.34) | |
| Premenopausal | ||||||
| Free | 1,124 | 5,594,895 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 118 | 384,776 | 1.43 (1.18, 1.73) | 1.43 (1.18, 1.73) | 1.30 (1.07, 1.57) | |
| Developed | 126 | 449,817 | 1.31 (1.09, 1.57) | 1.31 (1.09, 1.58) | 1.17 (0.97, 1.42) | |
| Persistent | 138 | 386,732 | 1.63 (1.36, 1.94) | 1.61 (1.34, 1.92) | 1.41 (1.17, 1.70) | |
| Perimenopausal | ||||||
| Free | 289 | 1,450,028 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 43 | 159,890 | 1.31 (0.95, 1.80) | 1.36 (0.98, 1.88) | 1.27 (0.92, 1.77) | |
| Developed | 48 | 191,356 | 1.23 (0.90, 1.67) | 1.29 (0.95, 1.75) | 1.19 (0.87, 1.63) | |
| Persistent | 64 | 187,006 | 1.64 (1.25, 2.16) | 1.75 (1.32, 2.31) | 1.59 (1.19, 2.12) | |
| Postmenopausal | ||||||
| Free | 1,155 | 9,383,793 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| Recovered | 321 | 2,259,422 | 1.30 (1.140, 1.47) | 1.36 (1.20, 1.54) | 1.24 (1.09, 1.40) | |
| Developed | 306 | 2,256,375 | 1.22 (1.07, 1.39) | 1.28 (1.13, 1.46) | 1.14 (1.00, 1.30) | |
| Persistent | 566 | 3,390,290 | 1.59 (1.43, 1.76) | 1.70 (1.53, 1.89) | 1.47 (1.32, 1.63) | |
Values are presented as hazard ratio (95% confidence interval).
1 Model 1 was adjusted for age at screening.
2 Model 2 was adjusted for age at screening, age at menarche, child delivery, breastfeeding, oral contraceptive use, family history of breast cancer, vigorous or moderate physical activity, smoking status, alcohol consumption, and breast density; For perimenopausal and postmenopausal women, the model was additionally adjusted for age at menopause and the use of hormone replacement therapy.
3 Model 3 was adjusted for covariates similar to model 2, with the addition of body mass index.
| Changes in MetS | No. of cases | Person-years | Model 11 | Model 22 | ||
|---|---|---|---|---|---|---|
| Non-obese (BMI <25.0 kg/m2) | ||||||
| Total | ||||||
| Free | 1,950 | 13,129,559 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 180 | 1,376,020 | 1.05 (0.90, 1.23) | 1.08 (0.92, 1.26) | ||
| Developed | 229 | 1,538,282 | 1.17 (1.02, 1.34) | 1.20 (1.04, 1.38) | ||
| Persistent | 180 | 1,322,467 | 1.17 (1.00, 1.37) | 1.22 (1.04, 1.43) | ||
| Premenopausal | ||||||
| Free | 899 | 4,727,718 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 40 | 171,897 | 1.11 (0.81, 1.53) | 1.13 (0.83, 1.56) | ||
| Developed | 59 | 229,162 | 1.24 (0.95, 1.62) | 1.26 (0.97, 1.65) | ||
| Persistent | 23 | 98,465 | 1.07 (0.70, 1.61) | 1.09 (0.72, 1.65) | ||
| Perimenopausal | ||||||
| Free | 229 | 1,182,722 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 14 | 74,060 | 0.91 (0.53, 1.56) | 0.94 (0.55, 1.62) | ||
| Developed | 24 | 100,176 | 1.18 (0.77, 1.79) | 1.23 (0.81, 1.88) | ||
| Persistent | 13 | 54,455 | 1.09 (0.62, 1.93) | 1.16 (0.66, 2.05) | ||
| Postmenopausal | ||||||
| Free | 822 | 7,219,118 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 126 | 1,130,063 | 1.10 (0.91, 1.32) | 1.14 (0.94, 1.37) | ||
| Developed | 146 | 1,208,945 | 1.17 (0.98, 1.40) | 1.22 (1.02, 1.45) | ||
| Persistent | 144 | 1,169,547 | 1.26 (1.05, 1.51) | 1.34 (1.12, 1.60) | ||
| Obese (BMI ≥25.0 kg/m2) | ||||||
| Total | ||||||
| Free | 618 | 3,299,157 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 302 | 1,428,069 | 1.30 (1.13, 1.49) | 1.30 (1.13, 1.49) | ||
| Developed | 251 | 1,359,266 | 1.11 (0.96, 1.29) | 1.11 (0.96, 1.29) | ||
| Persistent | 588 | 2,641,561 | 1.47 (1.30, 1.65) | 1.47 (1.31, 1.65) | ||
| Premenopausal | ||||||
| Free | 225 | 867,177 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 78 | 212,879 | 1.39 (1.08, 1.80) | 1.39 (1.07, 1.79) | ||
| Developed | 67 | 220,655 | 1.16 (0.88, 1.52) | 1.15 (0.88, 1.51) | ||
| Persistent | 115 | 288,267 | 1.50 (1.20, 1.88) | 1.49 (1.19, 1.87) | ||
| Perimenopausal | ||||||
| Free | 60 | 267,306 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 29 | 85,830 | 1.51 (0.97, 2.35) | 1.53 (0.98, 2.39) | ||
| Developed | 24 | 91,180 | 1.18 (0.73, 1.89) | 1.19 (0.74, 1.92) | ||
| Persistent | 51 | 132,551 | 1.72 (1.18, 2.51) | 1.76 (1.21, 2.57) | ||
| Postmenopausal | ||||||
| Free | 333 | 2,164,675 | 1.00 (reference) | 1.00 (reference) | ||
| Recovered | 195 | 1,129,359 | 1.23 (1.03, 1.47) | 1.25 (1.05, 1.49) | ||
| Developed | 160 | 1,047,430 | 1.07 (0.89, 1.30) | 1.10 (0.91, 1.32) | ||
| Persistent | 422 | 2,220,743 | 1.42 (1.22, 1.64) | 1.46 (1.26, 1.69) | ||
Values are presented as hazard ratio (95% confidence interval).
MetS, metabolic syndrome; BMI, body mass index.
1 Model 1 was adjusted for age at screening, age at menarche, child delivery, breastfeeding, oral contraceptive use, family history of breast cancer, vigorous or moderate physical activity, smoking status, alcohol consumption, and breast density; For perimenopausal and postmenopausal women, the model was additionally adjusted for age at menopause and the use of hormone replacement therapy.
2 Model 2 was adjusted for covariates similar to model 1, with the addition of BMI.
- 1. Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 2008;28:629-636.ArticlePubMed
- 2. Kim Y, Nho SJ, Woo G, Kim H, Park S, Kim Y, et al. Trends in the prevalence and management of major metabolic risk factors for chronic disease over 20 years: findings from the 1998-2018 Korea National Health and Nutrition Examination Survey. Epidemiol Health 2021;43:e2021028.ArticlePubMedPMC
- 3. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209-249.ArticlePubMedPDF
- 4. Kang SY, Lee SB, Kim YS, Kim Z, Kim HY, Kim HJ, et al. Breast cancer statistics in Korea, 2018. J Breast Cancer 2021;24:123-137.ArticlePubMedPMCPDF
- 5. Hong Y, Lee S, Moon S, Sung S, Lim W, Kim K, et al. Projection of cancer incidence and mortality from 2020 to 2035 in the Korean population aged 20 years and older. J Prev Med Public Health 2022;55:529-538.ArticlePubMedPMCPDF
- 6. Ha HI, Chang HK, Park SJ, Lim J, Won YJ, Lim MC. The incidence and survival of cervical, ovarian, and endometrial cancer in Korea, 1999-2017: Korea Central Cancer Registry. Obstet Gynecol Sci 2021;64:444-453.ArticlePubMedPMCPDF
- 7. Kang MJ, Won YJ, Lee JJ, Jung KW, Kim HJ, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2019. Cancer Res Treat 2022;54:330-344.ArticlePubMedPMCPDF
- 8. Esposito K, Chiodini P, Capuano A, Bellastella G, Maiorino MI, Giugliano D. Metabolic syndrome and endometrial cancer: a meta-analysis. Endocrine 2014;45:28-36.ArticlePubMedPDF
- 9. Yang X, Wang J. The role of metabolic syndrome in endometrial cancer: a review. Front Oncol 2019;9:744.ArticlePubMedPMC
- 10. Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D. Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care 2012;35:2402-2411.PubMedPMC
- 11. Hallajzadeh J, Khoramdad M, Izadi N, Karamzad N, Almasi-Hashiani A, Ayubi E, et al. Metabolic syndrome and its components in premenopausal and postmenopausal women: a comprehensive systematic review and meta-analysis on observational studies. Menopause 2018;25:1155-1164.ArticlePubMed
- 12. Cao Z, Zheng X, Yang H, Li S, Xu F, Yang X, et al. Association of obesity status and metabolic syndrome with site-specific cancers: a population-based cohort study. Br J Cancer 2020;123:1336-1344.ArticlePubMedPMCPDF
- 13. Zhao P, Xia N, Zhang H, Deng T. The metabolic syndrome is a risk factor for breast cancer: a systematic review and meta-analysis. Obes Facts 2020;13:384-396.ArticlePubMedPMCPDF
- 14. Premenopausal Breast Cancer Collaborative Group, Schoemaker MJ, Nichols HB, Wright LB, Brook MN, Jones ME, et al. Association of body mass index and age with subsequent breast cancer risk in premenopausal women. JAMA Oncol 2018;4:e181771.ArticlePubMedPMC
- 15. Neuhouser ML, Aragaki AK, Prentice RL, Manson JE, Chlebowski R, Carty CL, et al. Overweight, obesity, and postmenopausal invasive breast cancer risk: a secondary analysis of the women’s health initiative randomized clinical trials. JAMA Oncol 2015;1:611-621.ArticlePubMedPMC
- 16. Zhang Y, Liu Z, Yu X, Zhang X, Lü S, Chen X, et al. The association between metabolic abnormality and endometrial cancer: a large case-control study in China. Gynecol Oncol 2010;117:41-46.ArticlePubMed
- 17. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209-249.ArticlePubMedPDF
- 18. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHISNSC), South Korea. Int J Epidemiol 2017;46:e15.ArticlePubMed
- 19. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: executive summary. Crit Pathw Cardiol 2005;4:198-203.PubMed
- 20. Kim S, Kwon S. Impact of the policy of expanding benefit coverage for cancer patients on catastrophic health expenditure across different income groups in South Korea. Soc Sci Med 2015;138:241-247.ArticlePubMed
- 21. Yang MS, Park M, Back JH, Lee GH, Shin JH, Kim K, et al. Validation of cancer diagnosis based on the National Health Insurance Service Database versus the National Cancer Registry Database in Korea. Cancer Res Treat 2022;54:352-361.ArticlePubMedPMCPDF
- 22. World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment; 2000 [cited 2022 Nov 12]. Available from: https://apps.who.int/iris/handle/10665/206936.
- 23. Hwang KT, Han KD, Oh S, Koo BK, Lee SK, Kim J, et al. Influence of metabolic syndrome on risk of breast cancer: a study analyzing nationwide data from Korean National Health Insurance Service. Cancer Epidemiol Biomarkers Prev 2020;29:2038-2047.ArticlePubMedPDF
- 24. Choi IY, Chun S, Shin DW, Han K, Jeon KH, Yu J, et al. Changes in metabolic syndrome status and breast cancer risk: a nationwide cohort study. Cancers (Basel) 2021;13:1177.ArticlePubMedPMC
- 25. Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol 2017;960:1-17.ArticlePubMed
- 26. Moore LL, Chadid S, Singer MR, Kreger BE, Denis GV. Metabolic health reduces risk of obesity-related cancer in Framingham study adults. Cancer Epidemiol Biomarkers Prev 2014;23:2057-2065.ArticlePubMedPMCPDF
- 27. Kabat GC, Kim MY, Lee JS, Ho GY, Going SB, Beebe-Dimmer J, et al. Metabolic obesity phenotypes and risk of breast cancer in postmenopausal women. Cancer Epidemiol Biomarkers Prev 2017;26:1730-1735.ArticlePubMedPMCPDF
- 28. Park YM, White AJ, Nichols HB, O’Brien KM, Weinberg CR, Sandler DP. The association between metabolic health, obesity phenotype and the risk of breast cancer. Int J Cancer 2017;140:2657-2666.ArticlePubMedPMCPDF
- 29. Wang L, Du ZH, Qiao JM, Gao S. Association between metabolic syndrome and endometrial cancer risk: a systematic review and meta-analysis of observational studies. Aging (Albany NY) 2020;12:9825-9839.ArticlePubMedPMC
- 30. Friedenreich CM, Biel RK, Lau DC, Csizmadi I, Courneya KS, Magliocco AM, et al. Case-control study of the metabolic syndrome and metabolic risk factors for endometrial cancer. Cancer Epidemiol Biomarkers Prev 2011;20:2384-2395.ArticlePubMedPDF
- 31. Park B. Associations between obesity, metabolic syndrome, and endometrial cancer risk in East Asian women. J Gynecol Oncol 2022;33:e35.ArticlePubMedPMCPDF
- 32. Shoff SM, Newcomb PA. Diabetes, body size, and risk of endometrial cancer. Am J Epidemiol 1998;148:234-240.ArticlePubMed
- 33. Lim MC, Won YJ, Ko MJ, Kim M, Shim SH, Suh DH, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea during 1999-2015. J Gynecol Oncol 2019;30:e38.ArticlePubMedPMCPDF
- 34. Smith RA, von Eschenbach AC, Wender R, Levin B, Byers T, Rothenberger D, et al. American Cancer Society guidelines for the early detection of cancer: update of early detection guidelines for prostate, colorectal, and endometrial cancers. Also: update 2001--testing for early lung cancer detection. CA Cancer J Clin 2001;51:38-75.ArticlePubMed
- 35. Setiawan VW, Yang HP, Pike MC, McCann SE, Yu H, Xiang YB, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol 2013;31:2607-2618.ArticlePubMedPMC
- 36. Pfeiffer RM, Park Y, Kreimer AR, Lacey JV Jr, Pee D, Greenlee RT, et al. Risk prediction for breast, endometrial, and ovarian cancer in white women aged 50 y or older: derivation and validation from population-based cohort studies. PLoS Med 2013;10:e1001492.ArticlePubMedPMC
- 37. Stern T, Peleg Hasson S, Saad A, Levanon K, Michaan N, Laskov I, et al. Concomitant diagnosis of endometrial and breast cancer - does the sequence matters? Gynecol Oncol Rep 2021;38:100863.ArticlePubMedPMC
- 38. Hauner D, Hauner H. Metabolic syndrome and breast cancer: is there a link? Breast Care (Basel) 2014;9:277-281.ArticlePubMedPMCPDF
- 39. Bjørge T, Stocks T, Lukanova A, Tretli S, Selmer R, Manjer J, et al. Metabolic syndrome and endometrial carcinoma. Am J Epidemiol 2010;171:892-902.ArticlePubMed
- 40. Lindemann K, Vatten LJ, Ellstrøm-Engh M, Eskild A. Serum lipids and endometrial cancer risk: results from the HUNT-II study. Int J Cancer 2009;124:2938-2941.ArticlePubMed
- 41. Park SK. Epidemiological characteristics of breast cancer in Koreans. J Korean Med Assoc 2019;62:424-436 (Korean).ArticlePDF
REFERENCES
Figure & Data
References
Citations

- Metabolic Syndrome and Survival Outcomes in Endometrial Cancer
Alina-Gabriela Marin, Alexandru Filipescu, Radu Vladareanu, Aida Petca
Cureus.2024;[Epub] CrossRef - Melatonin, BAG-1 and cortisol circadian interactions in tumor pathogenesis and patterned immune responses
George Anderson
Exploration of Targeted Anti-tumor Therapy.2023; : 962. CrossRef - Changed Endocrinology in Postmenopausal Women: A Comprehensive View
Vidhi Motlani, Gunjan Motlani, Soumya Pamnani, Akshat Sahu, Neema Acharya
Cureus.2023;[Epub] CrossRef

 KSE
KSE


 PubReader
PubReader ePub Link
ePub Link Cite
Cite