Articles
- Page Path
- HOME > Epidemiol Health > Volume 45; 2023 > Article
-
COVID-19
Original Article
Parental concerns about COVID-19 vaccine safety and hesitancy in Korea: implications for vaccine communication -
Hye-Kyung Cho1*
 , Hyunju Lee2,3*
, Hyunju Lee2,3* , Young June Choe4
, Young June Choe4 , Shinkyeong Kim5
, Shinkyeong Kim5 , Sujin Seo5
, Sujin Seo5 , Jiwon Moon5
, Jiwon Moon5 , Eun Hwa Choi3
, Eun Hwa Choi3 , Geun-Yong Kwon6
, Geun-Yong Kwon6 , Jee Yeon Shin6
, Jee Yeon Shin6 , Sang-Yoon Choi6
, Sang-Yoon Choi6 , Mi Jin Jeong6
, Mi Jin Jeong6 , Myoungsoon You5
, Myoungsoon You5
-
Epidemiol Health 2022;45:e2023004.
DOI: https://doi.org/10.4178/epih.e2023004
Published online: December 13, 2022
1Department of Pediatrics, Ewha Womans University Mokdong Hospital, Seoul, Korea
2Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
3Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
4Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
5Department of Public Health Sciences, Graduate School of Public Health, Seoul National University, Seoul, Korea
6Division of Immunization, Korea Disease Control and Prevention Agency, Cheongju, Korea
- Correspondence: Myoungsoon You Department of Public Health Sciences, Graduate School of Public Health, Seoul National University, 1 Gwanak-ro, Gwanak-gu, Seoul 08826, Korea E-mail: msyou@snu.ac.kr
- *Cho & Lee contributed equally to this work as joint first authors.
© 2023, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
- Vaccination is one of the most important strategies to contain the spread of coronavirus disease 2019 (COVID-19). Vaccination in children is dependent on their parents, making it important to understand parents’ awareness and attitudes toward vaccines in order to devise strategies to raise vaccination rates in children.
-
METHODS
- A web-based nationwide survey was conducted among Korean parents of 7-year-old to 18-year-old children in August 2021 to estimate parents’ intention to vaccinate their children against COVID-19 and identify key factors affecting parental acceptance and hesitancy through regression analysis.
-
RESULTS
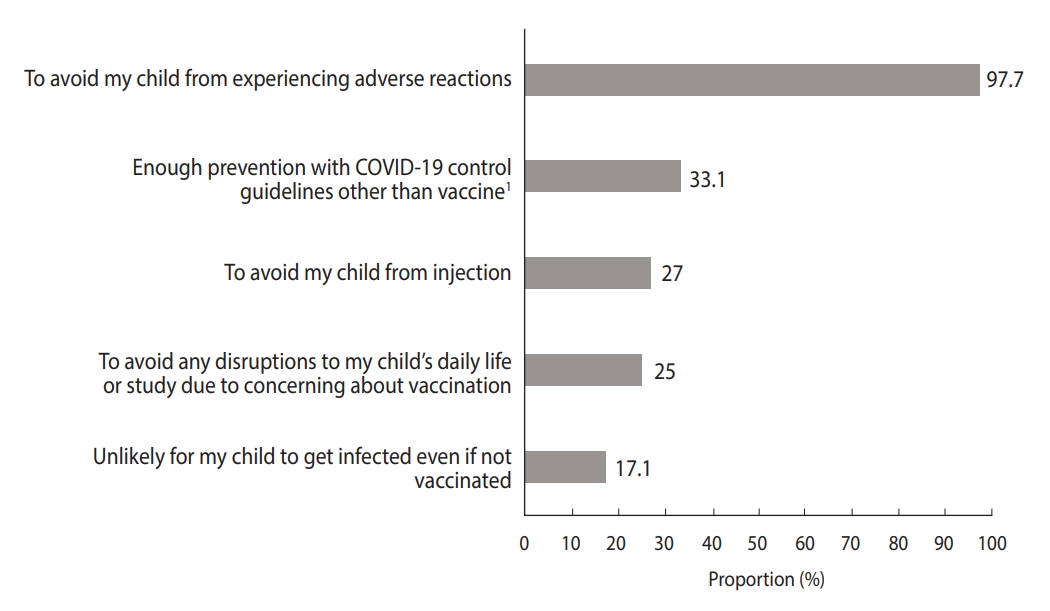
- Approximately 56.4% (575/1,019) were willing to vaccinate their children against COVID-19. Contributing factors to COVID-19 vaccine hesitancy were being a mother (adjusted odds ratio [aOR], 0.36; 95% confidence interval [CI], 0.25 to 0.52), a lower education level (aOR, 0.83; 95% CI, 0.70 to 0.97), hesitancy to other childhood vaccines (aOR, 0.78; 95% CI, 0.64 to 0.96), and refusal to vaccinate themselves (aOR, 0.08; 95% CI, 0.02 to 0.20). Having older children (aOR, 1.20; 95% CI, 1.13 to 1.28), trusting the child’s doctor (aOR, 1.19; 95% CI, 1.07 to 1.32), positive perceptions of the COVID-19 vaccine’s effectiveness (aOR, 2.60; 95% CI, 1.90 to 3.57) and perceiving the COVID-19 vaccine as low-risk (aOR, 1.68; 95% CI, 1.27 to 2.24) were associated with COVID-19 vaccine acceptance. Concerns about adverse reactions were the most common cause of hesitancy.
-
CONCLUSIONS
- Providing parents with accurate and reliable information on vaccine effectiveness and safety is important to increase COVID-19 vaccine uptake in children. Differential or targeted approaches to parents according to gender, age, and their children’s age are necessary for effective communication about vaccination in children.
- Keywords: SARS-CoV-2, COVID-19 vaccines, Child, Adolescents
- Vaccination is one of the most important strategies to control the ongoing coronavirus disease 2019 (COVID-19) pandemic. After COVID-19 vaccination began in adults in December 2020, vaccination in children under 16 years of age began in May 2021. However, there have been issues regarding the COVID-19 vaccine in that it uses a new platform and was developed in a relatively short period of time. In children, COVID-19 infection is known to have a relatively mild clinical course, but there have been reports of children with serious conditions or death [1,2]. In addition, the need for children’s COVID-19 vaccination is growing due to the contribution of the pediatric population, which makes up approximately 15-20% of the total population, to the spread of the virus in the community and indirect damages to children caused by prolonged social distancing or school closure during the pandemic. Therefore, careful decisions and approaches are required for pediatric COVID-19 vaccination policies.
- Some studies have been conducted in different countries on parental perceptions of children’s COVID-19 vaccination [3-8], finding that parental acceptance of COVID-19 vaccine for their children differs among countries and depends on factors such as parental age, geographic location, ethnicity, household income, acceptance of other childhood vaccines, perceived susceptibility to and risk of COVID-19, and perceived vaccine safety and effectiveness. Korean parents have historically had a very high acceptance of childhood vaccinations, resulting in high vaccination rates [9]. However, since the introduction of the COVID-19 vaccine, various issues regarding the safety of the vaccine have been raised, resulting in negative perceptions of the vaccine [10]. Given the lower parental acceptance of the COVID-19 vaccine for children compared to other childhood vaccines [11], it is necessary to further investigate factors related to parental willingness for their children to be vaccinated against COVID-19.
- Higher vaccine coverage is essential for improving the effectiveness of vaccines. To establish vaccination policies and strategies for this purpose, strategic communication between those to be vaccinated and policymakers should be devised based on an understanding of parents’ attitudes toward the vaccine and its contributing factors. This study aimed to analyze parental intentions to vaccinate their children against COVID-19 in Korea and factors influencing their attitudes, and to identify points to consider for improving vaccine coverage.
INTRODUCTION
- Study subjects and survey methods
- The cross-sectional web-based survey was performed among Korean parents of 7-year-old to 18-year-old children (first to 12th grades) across the country from August 11 to August 24, 2021, when COVID-19 vaccines were available only among adults aged ≥ 50 years and those with high-risk occupations in Korea. The survey was distributed via e-mail to a nationwide panel through a survey company. The subjects were selected by a proportional allocation extraction method by region, gender, age, and their child’s school and grade in school; elementary school (first to sixth grades), middle school (seventh to ninth grades) and high school (10th to 12th grades). Data such as demographic factors, child’s factors, perceptions of COVID-19 and COVID-19 vaccine, and their intention to vaccinate themselves and their children were collected. If a parent had multiple children, he or she was asked to choose only 1 and respond only regarding that child. The study was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies [12].
- Questionnaire development
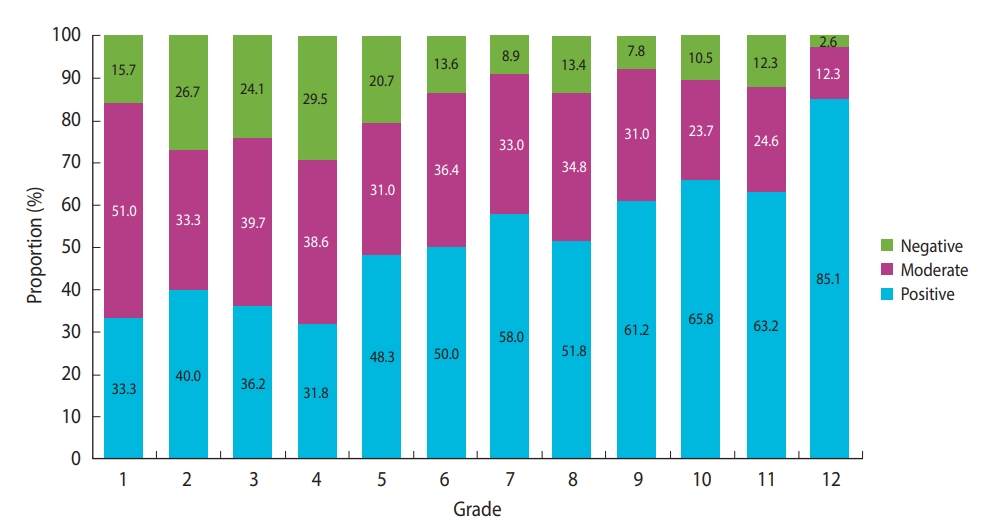
- The survey included questions based on previous surveys about perceptions of vaccination [5,6], with the development of multiple additional questions. The questions were organized into the following categories: demographic information of parents and children, parents’ intention to vaccinate themselves and their children against COVID-19, acceptance of past childhood vaccinations (including flu vaccines in the last 5 years), trust in the child’s doctors, the impact of COVID-19 on daily life, perceptions of the COVID-19 vaccine, and reasons affecting parents’ intention to vaccinate their children against COVID-19. The subjects’ residence was classified into Seoul, Gyeonggi Province, and Incheon as the metropolitan region, and other cities and provinces as the non-metropolitan region. Parental acceptance of vaccinating their child was classified into the following 3 categories: “very unlikely” and “less likely” were categorized as “negative,” “undecided” as “moderate,” and “likely” and “very likely” as “positive.” Those who reported “positive” acceptance were asked to choose 2 reasons why they were likely to vaccinate their child against COVID-19, and those who reported “moderate” and “negative” acceptance were prompted to choose 2 reasons why they were unlikely to vaccinate their child.
- Regarding the expected impact of getting COVID-19, participants were asked to answer a question (“If your child gets COVID-19, how serious do you think the impact [damage or loss] will be on the child’s health and daily life?”), with options including “very serious,” “serious,” “neutral,” “not serious,” or “not a problem.” They were also asked to answer a question about the expected risk of getting COVID-19 (“How likely do you think your child is to contract COVID-19?”), with possible responses of “very unlikely,” “unlikely,” “likely,” or “very likely.” They were also asked to select any of the following experiences that they had with COVID-19 among “my family members or I have been infected,” “my family members or I have been isolated as close contacts,” “my child’s school (or academy) teacher or friend has been infected,” “my child’s school (or academy) teacher or friend has been quarantined as a close contact,” and/or “not applicable.”
- Participants were asked to answer a question about parental behaviors toward seasonal influenza vaccine (“How have you been immunizing your child against seasonal influenza within the last 5 years?”), with options including “vaccinated every year,” “vaccinated 2‒3 times,” “vaccinated at least once,” or “never vaccinated” within 5 years or “can’t remember whether or not vaccinated.” Next, they were asked to answer a question about parents’ hesitancy to other childhood vaccines (“How much do you hesitate about other childhood vaccines in general?”), with the following possible options: “never hesitate,” “do not hesitate,” “do not know,” “hesitate,” or “strongly hesitate.” They were asked to choose an option on a scale from 0 (not trust him/her at all) to 10 (trust him/her very much) regarding their trust in their child’s primary care physician.
- Participants were asked to answer a question about their intention to vaccinate themselves against COVID-19 (“Would you have yourself vaccinated against COVID-19 if available?”), with possible responses including “definitely,” “probably,” “probably not,” “never,” “I don’t know,” or “already done.” They were also asked to choose an answer (“strongly agree,” “agree,” “neither agree nor disagree,” “disagree,” or “strongly disagree”) for the following statements: “the COVID-19 vaccine is safe for me (perceived safety of COVID-19 vaccine),” “the COVID-19 vaccine is effective to prevent infection, serious illness, and death (perceived effectiveness of the vaccine),” and “the possibility that adverse reactions occur after COVID-19 vaccination is low (perceived risk of the vaccine).”
- Statistical analysis
- Descriptive statistics (i.e., frequencies and percentages for categorical variables, mean and standard deviation [SD] for continuous variables) were performed for the independent variables. We then assessed the associations between parents’ intention to vaccinate their children against COVID-19 and the independent variables using the chi-square test and multivariate logistic regression, reporting adjusted odds ratios (aORs) with 95% confidence intervals (CIs).
- The predictive variables included in the logistic regression were characteristics commonly associated with vaccination hesitancy from the previous literature. Cases with missing data were excluded from the analysis.
- To assess the predictors of parental intention to vaccinate their children against COVID-19, the associations between the variables and parental intention were analyzed using multivariate logistic regression analysis with R version 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria).
- Ethics statement
- This survey was conducted with support from the Korea Disease Control and Prevention Agency to be utilized in developing comprehensive vaccination policies for children. This study was performed with approval from the Korea University Institutional Review Board (protocol No. 2021AN0402).
MATERIALS AND METHODS
- Demographic characteristics of participants
- A total of 1,025 parents participated in the survey, although 6 participants were excluded due to incomplete responses. Among 1,019 parents who completed the survey, 57.6% of the respondents were women, and most of them were in their 40s. The area of residence (metropolitan and non-metropolitan region), gender, and children’s school level (elementary, middle, and high school) were evenly distributed. Other factors collected included the parent’s education, monthly household income, child’s health condition and flu shot vaccination rate (for at least 1 shot during the past 5 years). Socio-demographic factors of the parents and their children are presented in Table 1.
- COVID-19 vaccine acceptance and contributing factors
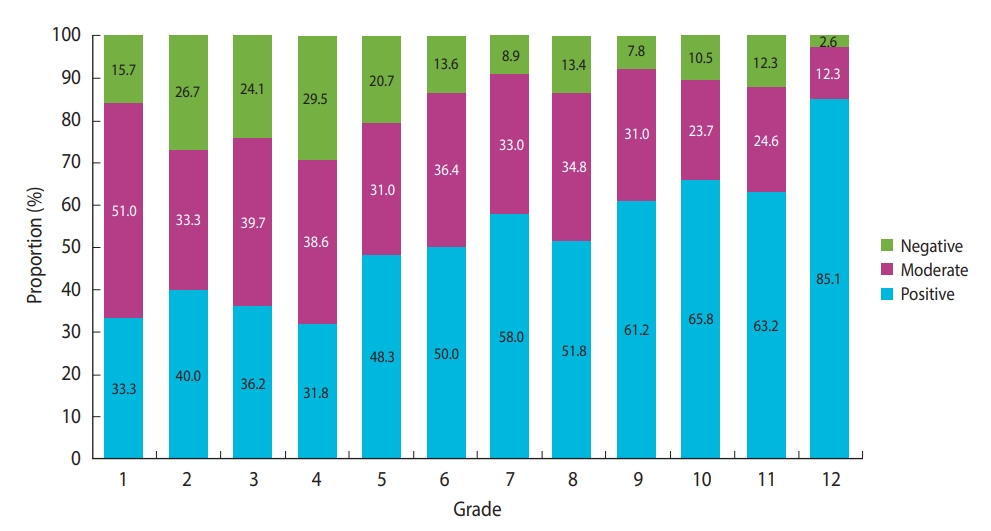
- The overall COVID-19 vaccine acceptance rate among parents of children in the first to 12th grades was 56.4%. Hesitancy was higher among mothers than among fathers. COVID-19 vaccine acceptance for children was lower in younger parents and parents with younger children (Table 2 and Figure 1). Low household income was also related to COVID-19 vaccine hesitancy. However, the expected impact on the child’s health and daily life from getting COVID-19 and the expected risk of the child contracting COVID-19 did not affect parental intentions to vaccinate their children. Experiences of being infected with or exposed to COVID-19, also did not affect parents’ intentions to vaccinate their child. Recent flu shot uptake for children in the past 5 years, which was high (92.2%), did not affect parental attitudes toward COVID-19 vaccination for their children, although respondents who showed hesitancy toward other childhood vaccines had lower acceptance of the COVID-19 vaccine than those who had not. Although 85.0% of the parents answered that they trusted their child’s doctor, those who did not trust their child’s doctor had lower acceptance of their child’s COVID-19 vaccine compared to those with trust in their child’s doctor. Parents who were themselves already vaccinated or were willing to be vaccinated showed higher acceptance of the vaccination for their children than parents who were not willing to get vaccinated themselves. Awareness of the effectiveness, safety, and risk of the COVID-19 vaccine was found to affect parental acceptance of the COVID-19 vaccine for their children.
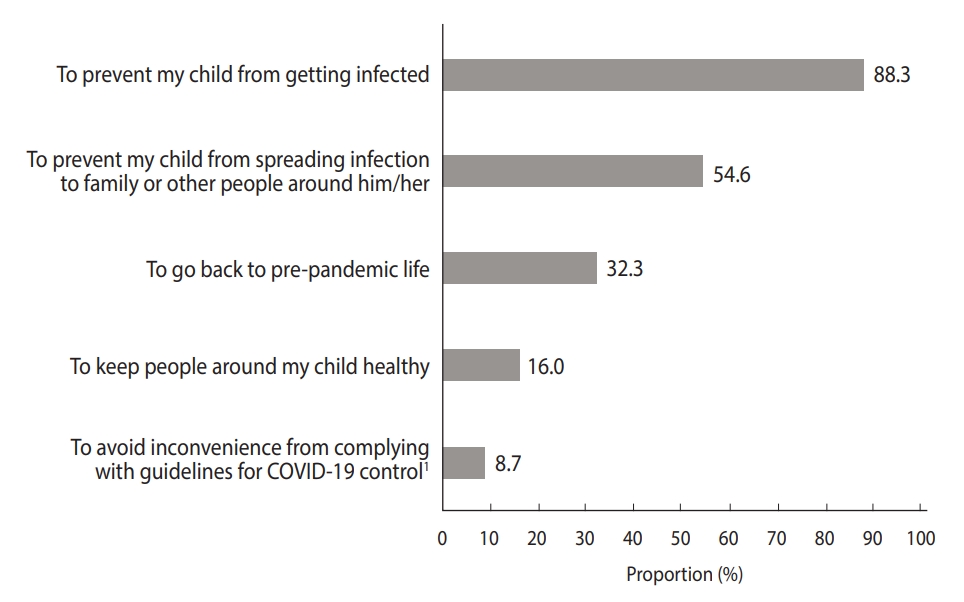
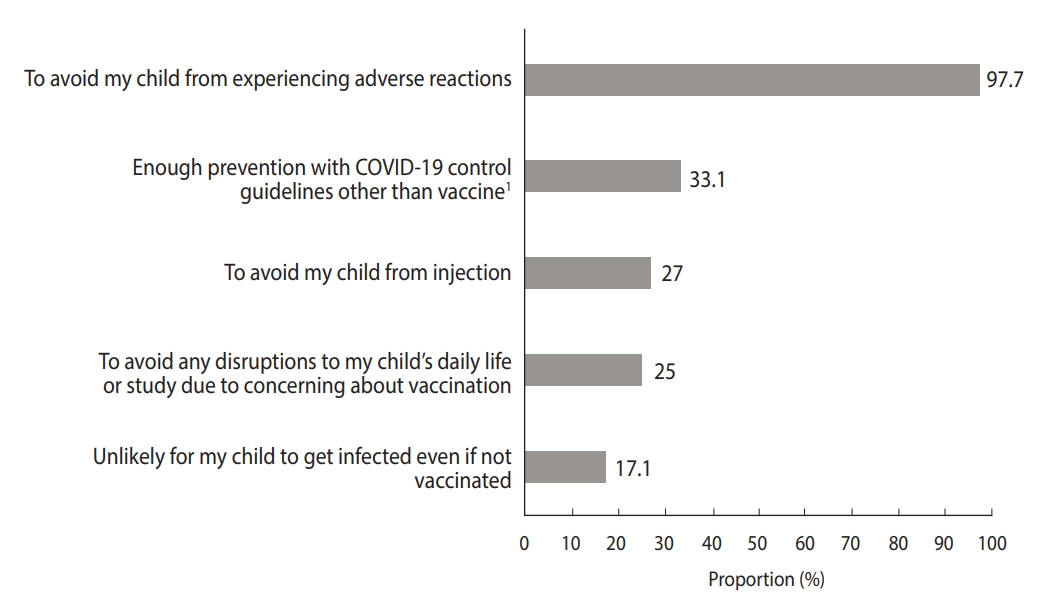
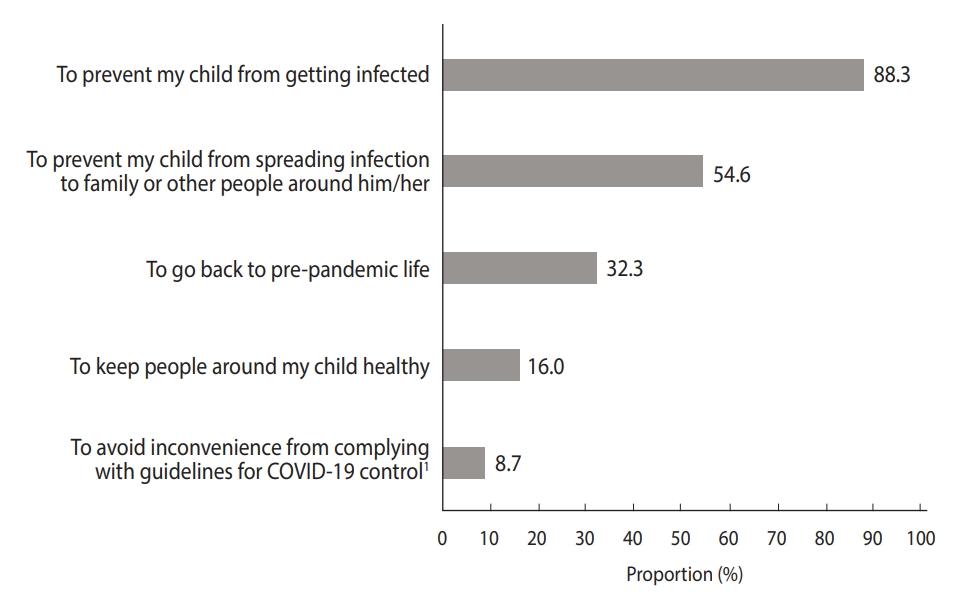
- The most common reason to have their children vaccinated was “to prevent my child from getting infected,” followed by “to prevent those around you from COVID-19” (Figure 2). Meanwhile, the most common reason to hesitate about the COVID-19 vaccine for their children was “to avoid my child from experiencing adverse reactions,” followed by “adhering to other COVID-19 control policies is sufficient to prevent it” (Figure 3).
- Multivariate analysis of parents’ intention to vaccinate their children against COVID-19
- The predictors of parents’ intention to vaccinate their children with COVID-19 vaccine were analyzed using multivariate binary logistic regression (Table 3). Being a mother (aOR, 0.36; 95% CI, 0.25 to 0.52), lower parental education levels (aOR, 0.83; 95% CI, 0.70 to 0.97), hesitancy toward other childhood vaccines (aOR, 0.78; 95% CI, 0.64 to 0.96) and a lack of parental willingness to be vaccinated themselves (aOR, 0.08; 95% CI, 0.02 to 0.20) were associated with lower parental intention to have their children vaccinated. Older children (aOR, 1.20; 95% CI, 1.13 to 1.28), trust in doctors (aOR, 1.19; 95% CI, 1.07 to 1.32), positive perceptions of the effectiveness of the COVID-19 vaccine (aOR, 2.60; 95% CI, 1.90 to 3.57), and considering the COVID-19 vaccine to be low-risk (aOR, 1.68; 95% CI, 1.27 to 2.24) were associated with parental acceptance of vaccinating their children.
RESULTS
- In this in-depth survey of parents of children 7-18 years of age, we analyzed parental acceptance of COVID-19 vaccination in children. This study helps to elucidate and better understand parental COVID-19 vaccine hesitancy for their children and its associated factors. According to the results, COVID-19 vaccine hesitancy was related to women gender, lower parental education, younger children, hesitancy toward other childhood vaccines, lack of trust in the child’s doctor, parental intention not to receive the vaccination themselves, and negative parental perceptions of the vaccine’s effectiveness and risks.
- Parental intention to vaccinate their child against COVID-19 differs by country, the time of the survey, race/ethnicity, parental age, gender and educational level, children’s age, parental attitudes toward being vaccinated themselves, and experiences with COVID-19 [3,4,6,13-19]. In this study, factors affecting parental intention to vaccinate children included the age and gender of parents, the parents’ education level, the children’s age, and parental attitudes toward receiving the vaccination themselves, which is consistent with most studies from different countries [15,18,19]. Of note, parents of younger children were less likely to have their children vaccinated even if they had already been vaccinated or were willing to be vaccinated themselves. This finding suggests that parents seem to expect greater standards of safety profiles from vaccines for younger children. Parents of younger children may have more concern about potential long-term adverse effects, which was also the most important factor of vaccine hesitancy in many other studies [4,6,18-20]. This finding could be related to the widely known fact that younger adults or children with COVID-19 have mild symptoms and clinical courses [7]. Previous studies have reported that personal experience with COVID-19 affected parents’ attitudes toward vaccination [17,21,22]. A survey conducted in the United States showed that parental intention to vaccinate their child was associated with knowing someone who died of COVID-19 [15]. In this study, however, experiences of family members or the child’s friends or teachers being quarantined after being infected with or coming into contact with COVID-19 were not factors that affected the intention to vaccinate. It seems that the impact of experiences with COVID-19 on the intention to vaccinate may depend on the type (e.g., being infected or being quarantined) and severity (e.g., asymptomatic, severe illness, or death) of the experience.
- As shown in other studies, parental perceptions of vaccine safety and adverse reactions were the most important factors associated with a positive intention to vaccinate in this study [23]. In addition, most parents answered that the reason for their hesitancy to have their children vaccinated against COVID-19 was “to avoid my child from experiencing adverse reactions.” Most studies have consistently shown that concerns about adverse reactions to the vaccine and unknown long-term adverse effects are the most influential factors for parental hesitancy toward the COVID-19 vaccine [13,15,18,19]. In particular, as the number of people who access information about vaccines through social media and internet messages increases, there are growing concerns regarding misinformation or mistrust about vaccines from unreliable sources [4,24-26]. This suggests that providing reliable information on vaccine safety should be considered as a top priority. Some studies have emphasized the role of physicians or health care providers in communication with parents about children’s COVID-19 vaccination [6] and others reinforced the need for health authorities to take the lead in providing knowledge about COVID-19 vaccine, along with transparent information related to adverse reactions associated with this vaccination [13,14].
- In this cross-sectional survey, which was conducted in August 2021, when 41.6% of the total Korean population had received at least 1 dose of the vaccine (15.4% had completed the vaccination series), 56.4% of Korean parents reported acceptance of the COVID-19 vaccine for their children. Although studies on the intention of Korean parents to have their children vaccinated against COVID-19 are very limited, a study showed that 64.2% of the parents intended to vaccinate their children, which was higher than that in this study [16]. The higher acceptance rate observed in the previous study might be explained by the fact that it was hospital-based and the participants were likely to be at an elevated risk for severe COVID-19. In another Korean study that was performed in December 2021, when most adults had completed their vaccination series in Korea, 34.2% of parents reported acceptance of the COVID-19 vaccine for their child [27]. Therefore, acceptance rates may fluctuate across different time points and epidemic waves according to parents’ experiences and information about adverse reactions or breakthrough infections, which is consistent with other survey-based research performed before and after the implementation of COVID vaccination [18]. Therefore, it is necessary to continue monitoring changes in parental intentions to improve vaccination rates.
- In Korea, the mRNA vaccine for children aged 12-15 years and those aged 5-11 years has been available since November 1, 2021 (October 18, 2021 for those aged 16-17 years) and March 31, 2022, respectively [28,29]. As of December 31, 2021, 74.0% of children aged 12-17 years in Korea had received at least one dose of the vaccine [30], which was higher than the percentage of parents who intended to vaccinate their children in this survey (56.0% in 12-15 year-olds and 71.3% in ≥ 16 year-olds). This might have been because more safety information was collected from Korea and other countries for about 4 months after the survey. The increase in vaccination among friends and family members may have contributed to the increased uptake of the COVID-19 vaccine in children 12-17 years of age. Furthermore, in early December 2021, the Korean government announced that it would apply the quarantine pass for entrance to private academies and study rooms starting in March 2022, which seems to have had a major impact on raising the vaccination rate in this age group. The vaccination rate has risen during the winter break as children and parents may prefer to avoid disruptions to schoolwork and prepare for the new school year, which starts in March. However, as of May 9, 2022, the vaccination rate for children aged 5-11 in Korea was 1.3%, much lower than the rate that would be expected from this study (38.4% in ≤ 11-year-olds) as well as than that of other countries (e.g., 20% in Germany, 35% in the United States, and 57% in Spain) [31,32]. This may have resulted from the relatively low severity of COVID-19 in young children and the waning vaccine effectiveness during the Omicron surge with rising breakthrough infections since the end of January 2022 in Korea. However, the significant difference in the vaccination rate between children aged 12-17 years and those aged 5-11 years may also reflect a disparity in parents’ perceptions of vaccine-related adverse reactions. As seen in our regression analysis, parents’ perception of the vaccine safety did not differ between the acceptance group and the hesitancy group, but concerns about adverse reactions had a negative effect on parents’ intention to vaccinate their children. This finding has been consistently observed in other studies as well [18,19], which means that concerns about adverse reactions do not simply reflect misinformation that can be solved by educating parents about vaccine safety; instead, some hesitancy originates intuitively from persistent psychological traits [33]. Since this psychological reactance is likely to affect parents of younger children, makes communication with physicians less effective, and results in hesitancy toward vaccination [34-36], alternative communication strategies tailored to this population are required.
- This study has some limitations. Because this study was conducted among the parents of elementary, middle, and high school students (7-18 year-olds) in Korea, the parents of 12th graders, approximately 95% of whom had already been vaccinated at the time of the survey, were included. As a result, overall parental willingness may have been overestimated in this study compared to the actual percentage of parents who intended to have their children vaccinated.
- Despite these limitations, this study provides important information on parents’ perceptions of the COVID-19 vaccine, their intention to vaccinate their children, and factors related to their attitudes. These findings help to devise strategies to overcome hesitancy toward the vaccine and improve vaccine coverage in children. This study also has the advantage that the subjects were enrolled nationwide and evenly by region and age, making it possible to conduct a survey representing parents across the country.
- Approximately half of Korean parents intended to vaccinate their children against COVID-19, and higher hesitancy was shown in younger children’s parents. Parents’ concerns about experiencing adverse reactions were the largest factor affecting awareness and attitudes toward COVID-19 vaccination for their children, which is consistent with previous studies. Strategies to provide parents with accurate and reliable vaccine information will be important to increase the uptake of COVID-19 vaccination in children. Differential or targeted approaches to parents according to gender, age, and the age of their children may also be necessary for effective communication to mitigate parents’ concerns about COVID-19 vaccination in children.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare for this study.
-
FUNDING
This research was funded by the Korea Disease Control and Prevention Agency (No. 2021-10-023).
-
AUTHOR CONTRIBUTIONS
Conceptualization: Lee H, Choi EH, You M, Choe YJ. Data curation: Kim S, Seo S, Moon J. Formal analysis: Cho HK, Lee H. Funding acquisition: Choe YJ, Choi EH. Methodology: You M, Kwon GY, Shin JY, Choi SY, Jeong MJ. Writing – original draft: Cho HK, Lee H. Writing – review & editing: Choe YJ, Kim S, Seo S, Moon J, Choi EH, Kwon GY, Shin JY, Choi SY, Jeong MJ, You M.
NOTES
ACKNOWLEDGEMENTS
| Variables | aOR (95% CI) | p-value |
|---|---|---|
| Gender, women (ref: men) | 0.36 (0.25, 0.52) | <0.001 |
| Age | 1.04 (0.99. 1.09) | 0.069 |
| Residence non-metropolitan (ref: metropolitan) | 0.94 (0.68, 1.28) | 0.678 |
| Education | 0.83 (0.70, 0.97) | 0.023 |
| Monthly household income | 1.08 (0.99, 1.18) | 0.054 |
| Child’s gender, women (ref: men) | 1.04 (0.76, 1.42) | 0.803 |
| Child’s age | 1.20 (1.13, 1.28) | <0.001 |
| Child’s health condition | 1.11 (0.89, 1.39) | 0.361 |
| Expected impact on child’s health and daily life from getting COVID-19 | 1.17 (0.95, 1.44) | 0.147 |
| Expected risk of getting COVID-19 | 1.01 (0.83, 1.24) | 0.891 |
| COVID-19 experiences, yes (ref: no)1 | 0.90 (0.65, 1.24) | 0.509 |
| Flu shot uptake in the last 5 yr, yes (ref: no) | 1.04 (0.57, 1.90) | 0.902 |
| Hesitancy toward other childhood vaccines | 0.78 (0.64, 0.96) | 0.017 |
| Trust in the child’s doctor | 1.19 (1.07, 1.32) | 0.001 |
| Parental intention to be vaccinated themselves, hesitancy (ref: accept) | 0.08 (0.02, 0.20) | <0.001 |
| Perceived safety of the COVID-19 vaccine | 1.06 (0.78, 1.43) | 0.721 |
| Perceived effectiveness of the COVID-19 vaccine | 2.60 (1.90, 3.57) | <0.001 |
| Perceived risk of the COVID-19 vaccine, low | 1.68 (1.27, 2.24) | <0.001 |
All variables except variables with reference categories were included in the regression analysis as continuous variables.
COVID-19, coronavirus disease 2019; aOR, adjusted odds ratio; CI, confidence interval; ref, reference value.
1 COVID-19 infection and exposure of family members, child’s teachers or friends, yes (ref = no).
- 1. Preston LE, Chevinsky JR, Kompaniyets L, Lavery AM, Kimball A, Boehmer TK, et al. Characteristics and disease severity of us children and adolescents diagnosed with COVID-19. JAMA Netw Open 2021;4:e215298.ArticlePubMedPMC
- 2. Lee H, Choi S, Park JY, Jo DS, Choi UY, Lee H, et al. Analysis of critical COVID-19 cases among children in Korea. J Korean Med Sci 2022;37:e13.ArticlePubMedPDF
- 3. Humble RM, Sell H, Dubé E, MacDonald NE, Robinson J, Driedger SM, et al. Canadian parents’ perceptions of COVID-19 vaccination and intention to vaccinate their children: results from a crosssectional national survey. Vaccine 2021;39:7669-7676.ArticlePubMedPMC
- 4. Horiuchi S, Sakamoto H, Abe SK, Shinohara R, Kushima M, Otawa S, et al. Factors of parental COVID-19 vaccine hesitancy: a cross sectional study in Japan. PLoS One 2021;16:e0261121.ArticlePubMedPMC
- 5. Ruggiero KM, Wong J, Sweeney CF, Avola A, Auger A, Macaluso M, et al. Parents’ intentions to vaccinate their children against COVID-19. J Pediatr Health Care 2021;35:509-517.ArticlePubMedPMC
- 6. Szilagyi PG, Shah MD, Delgado JR, Thomas K, Vizueta N, Cui Y, et al. Parents’ intentions and perceptions about COVID-19 vaccination for theirchildren: results from a national survey. Pediatrics 2021;148:e2021052335.ArticlePubMedPDF
- 7. Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine 2020;38:7789-7798.ArticlePubMedPMC
- 8. Lackner CL, Wang CH. Demographic, psychological, and experiential correlates of SARS-CoV-2 vaccination intentions in a sample of Canadian families. Vaccine X 2021;8:100091.ArticlePubMedPMC
- 9. Yu JH, Jeong HJ, Kim SJ, Lee JY, Choe YJ, Choi EH, et al. Sustained vaccination coverage during the coronavirus disease 2019 epidemic in the Republic of Korea. Vaccines (Basel) 2020;9:2.ArticlePubMedPMC
- 10. Lee H, Noh EB, Park SJ, Nam HK, Lee TH, Lee GR, et al. COVID-19 vaccine perception in South Korea: web crawling approach. JMIR Public Health Surveill 2021;7:e31409.ArticlePubMedPMC
- 11. Lee H, Choe YJ, Kim S, Cho HK, Choi EH, Lee J, et al. Attitude and acceptance of COVID-19 vaccine in parents and adolescents: a nationwide survey. J Adolesc Health 2022;71:164-171.ArticlePubMedPMC
- 12. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344-349.ArticlePubMed
- 13. Xu Y, Xu D, Luo L, Ma F, Wang P, Li H, et al. A cross-sectional survey on COVID-19 vaccine hesitancy among parents from Shandong vs. Zhejiang. Front Public Health 2021;9:779720.ArticlePubMedPMC
- 14. Temsah MH, Alhuzaimi AN, Aljamaan F, Bahkali F, Al-Eyadhy A, Alrabiaah A, et al. Parental attitudes and hesitancy about COVID-19 vs. routine childhood vaccinations: a national survey. Front Public Health 2021;9:752323.ArticlePubMedPMC
- 15. Rane MS, Robertson MM, Westmoreland DA, Teasdale CA, Grov C, Nash D. Intention to vaccinate children against COVID-19 among vaccinated and unvaccinated US parents. JAMA Pediatr 2022;176:201-203.ArticlePubMed
- 16. Choi SH, Jo YH, Jo KJ, Park SE. Pediatric and parents’ attitudes towards COVID-19 vaccines and intention to vaccinate for children. J Korean Med Sci 2021;36:e227.ArticlePubMedPMCPDF
- 17. Altulaihi BA, Alaboodi T, Alharbi KG, Alajmi MS, Alkanhal H, Alshehri A. Perception of parents towards COVID-19 vaccine for children in Saudi population. Cureus 2021;13:e18342.ArticlePubMedPMC
- 18. Zhou X, Wang S, Zhang K, Chen S, Chan PS, Fang Y, et al. Changes in parents’ COVID-19 vaccine hesitancy for children aged 3-17 years before and after the rollout of the national childhood COVID-19 vaccination program in China: repeated cross-sectional surveys. Vaccines (Basel) 2022;10:1478.ArticlePubMedPMC
- 19. Yoda T, Katsuyama H. Parents’ hesitation about getting their children vaccinated against COVID-19 in Japan. Hum Vaccin Immunother 2021;17:4993-4998.ArticlePubMedPMC
- 20. Alhazza SF, Altalhi AM, Alamri KM, Alenazi SS, Alqarni BA, Almohaya AM. Parents’ hesitancy to vaccinate their children against COVID-19, a country-wide survey. Front Public Health 2022;10:755073.ArticlePubMedPMC
- 21. Gönüllü E, Soysal A, Atıcı S, Engin M, Yeşilbaş O, Kasap T, et al. Pediatricians’ COVID-19 experiences and views on the willingness to receive COVID-19 vaccines: a cross-sectional survey in Turkey. Hum Vaccin Immunother 2021;17:2389-2396.ArticlePubMedPMC
- 22. Ellithorpe ME, Aladé F, Adams RB, Nowak GJ. Looking ahead: caregivers’ COVID-19 vaccination intention for children 5 years old and younger using the health belief model. Vaccine 2022;40:1404-1412.ArticlePubMedPMC
- 23. Shmueli L. Parents’ intention to vaccinate their 5-11 years old children with the COVID-19 vaccine: rates, predictors and the role of incentives. medRxiv [Preprint]; 2020 [cited 2022 Jul 20]. Available from: https://doi.org/10.1101/2021.11.05.21265900.Article
- 24. Suran M. Why parents still hesitate to vaccinate their children against COVID-19. JAMA 2022;327:23-25.ArticlePubMed
- 25. Islam MS, Kamal AM, Kabir A, Southern DL, Khan SH, Hasan SM, et al. COVID-19 vaccine rumors and conspiracy theories: the need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS One 2021;16:e0251605.ArticlePubMedPMC
- 26. Jennings W, Stoker G, Bunting H, Valgarðsson VO, Gaskell J, Devine D, et al. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines (Basel) 2021;9:593.ArticlePubMedPMC
- 27. Noh Y, Kim JH, Yoon D, Choe YJ, Choe SA, Jung J, et al. Predictors of COVID-19 booster vaccine hesitancy among fully vaccinated adults in Korea: a nationwide cross-sectional survey. Epidemiol Health 2022;44:e2022061.ArticlePubMedPMCPDF
- 28. Korea Disease Control and Prevention Agency. Current status of COVID-19 outbreak and vaccination in Korea (11.1.); 2021 [cited 2022 Jan 26]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=717408&cg_code=&act=view&nPage=27 (Korean).
- 29. Korea Disease Control and Prevention Agency. Current status of COVID-19 outbreak and vaccination in Korea (3.27.); 2022 [cited 2022 May 9]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=719114&cg_code=&act=view&nPage=11# (Korean).
- 30. Korea Disease Control and Prevention Agency. Current status of COVID-19 outbreak and vaccination in Korea (12.31.); 2021 [cited 2022 Feb 5]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=718152&cg_code=&act=view&nPage=31 (Korean).
- 31. American Academy of Pediatrics. Children and COVID-19 vaccination trends; 2022 [cited 2022 May 9]. Available from: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-vaccination-trends/.
- 32. Smith I. COVID vaccines: which countries are vaccinating children over 5 and how do they compare? Euronews; 2022 May 9 [cited 2022 May 9]. Available from: https://www.euronews.com/next/2022/02/25/covid-vaccine-for-children-who-in-europe-isleading-the-race.
- 33. Browne M, Thomson P, Rockloff MJ, Pennycook G. Going against the herd: psychological and cultural factors underlying the ‘vaccination confidence gap’. PLoS One 2015;10:e0132562.ArticlePubMedPMC
- 34. Finkelstein SR, Boland WA, Vallen B, Connell PM, Sherman GD, Feemster KA. Psychological reactance impacts ratings of pediatrician vaccine-related communication quality, perceived vaccine safety, and vaccination priority among U.S. parents. Hum Vaccin Immunother 2020;16:1024-1029.ArticlePubMed
- 35. Soveri A, Karlsson LC, Mäki O, Antfolk J, Waris O, Karlsson H, et al. Trait reactance and trust in doctors as predictors of vaccination behavior, vaccine attitudes, and use of complementary and alternative medicine in parents of young children. PLoS One 2020;15:e0236527.ArticlePubMedPMC
- 36. Woller KM, Buboltz WC Jr, Loveland JM. Psychological reactance: examination across age, ethnicity, and gender. Am J Psychol 2007;120:15-24.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Safety of BNT162b2 mRNA COVID-19 vaccine in children with chronic kidney disease: a national population study from South Korea
Young June Choe, Yo-Han Ahn, Eunsun Gwak, Eunseo Jo, Jinseob Kim, Seung-Ah Choe
Pediatric Nephrology.2024; 39(2): 625. CrossRef - Willingness and hesitancy of parents to vaccinate against COVID-19 their children ages 6 months to 4 years with frail conditions in Italy
Grazia Miraglia del Giudice, Giorgia Della Polla, Mario Postiglione, Italo Francesco Angelillo
Frontiers in Public Health.2023;[Epub] CrossRef

 KSE
KSE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite