Articles
- Page Path
- HOME > Epidemiol Health > Volume 44; 2022 > Article
-
Original Article
The predictive value of resting heart rate in identifying undiagnosed diabetes in Korean adults: Korea National Health and Nutrition Examination Survey -
Dong-Hyuk Park1
 , Wonhee Cho1
, Wonhee Cho1 , Yong-Ho Lee2
, Yong-Ho Lee2 , Sun Ha Jee3,4
, Sun Ha Jee3,4 , Justin Y. Jeon1,3
, Justin Y. Jeon1,3
-
Epidemiol Health 2022;44:e2022009.
DOI: https://doi.org/10.4178/epih.e2022009
Published online: January 3, 2022
1Department of Sports Industry, Yonsei University, Seoul, Korea
2Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
3Exercise Medicine Center for Diabetes and Cancer Patients, Institute of Convergence of Science (ICONS), Yousei university, Seoul, Korea
4Institute for Health Promotion, Graduate School of Public Health, Yonsei University, Seoul, Korea
- Correspondence: Justin Y. Jeon Department of Sports Industry, Yonsei University, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea E-mail: jjeon@yonsei.ac.kr
©2022, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
- The purpose of this study was (1) to examine whether the addition of resting heart rate (RHR) to the existing undiagnosed diabetes mellitus (UnDM) prediction model would improve predictability, and (2) to develop and validate UnDM prediction models by using only easily assessable variables such as gender, RHR, age, and waist circumference (WC).
-
METHODS
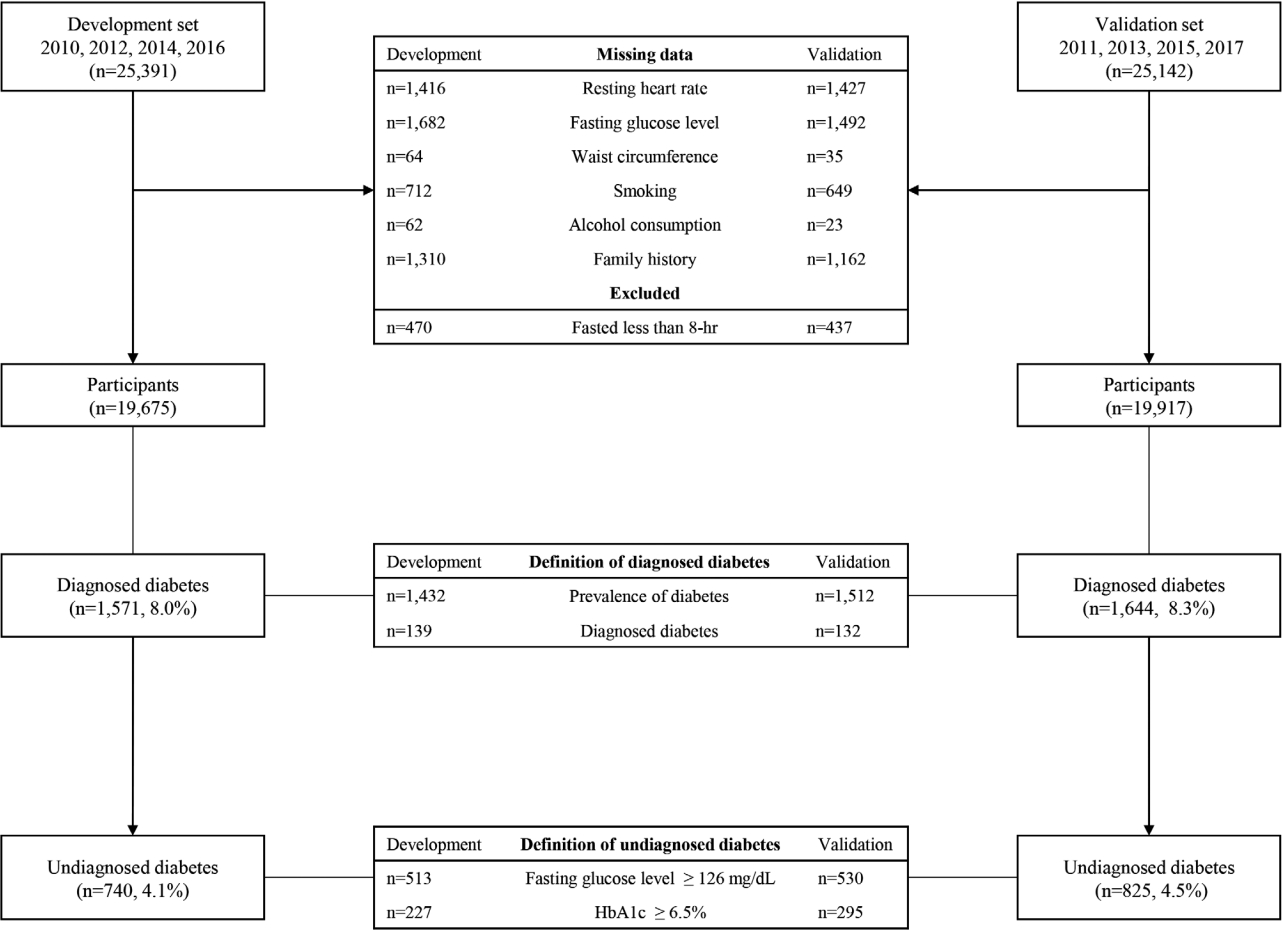
- Korea National Health and Nutrition Examination Survey (KNHANES) 2010, 2012, 2014, 2016 data were used to develop the model (model building set, n=19,675), while the data from 2011, 2013, 2015, 2017 were used to validate the model (validation set, n=19,917). UnDM was defined as a fasting glucose level ≥126 mg/dL or glycated hemoglobin ≥6.5%; however, doctors have not diagnosed it. Statistical package for the social sciences logistic regression analysis was used to determine the predictors of UnDM.
-
RESULTS
- RHR, age, and WC were associated with UnDM. When RHR was added to the existing model, sensitivity was reduced (86 vs. 73%), specificity was increased (49 vs. 65%), and a higher Youden index (35 vs. 38) was expressed. When only gender, RHR, age, and WC were used in the model, a sensitivity, specificity, and Youden index of 70%, 67%, and 37, respectively, were observed.
-
CONCLUSIONS
- Adding RHR to the existing UnDM prediction model improved specificity and the Youden index. Furthermore, when the prediction model only used gender, RHR, age, and WC, the outcomes were not inferior to those of the existing prediction model.
- According to the Korea National Health and Nutrition Examination Survey (KNHANES), the prevalence of diabetes in individuals over the age of 30 was 13.8%, which is equivalent to 4.94 million cases [1]. Diabetes is the sixth leading cause of mortality in Korea [2]. It is associated with complications such as cardiovascular disease [3], stroke [4], peripheral arterial diseases [5], increased mortality [6] and lowered quality of life [7]. However, the rate of undiagnosed diabetes is 21.4% in the Unite States and 35.0% in Korea, increasing every year [1,8].
- Undiagnosed diabetes leads to late treatment initiation, which increases risk of complications [9]. Therefore, early detection of undiagnosed diabetes is an important issue and therefore risk scores for undiagnosed diabetes are being developed worldwide, using the risk factors for diabetes [10-12]. In Korea, Lee et al. [12] developed a model with 80% sensitivity, 53% specificity, 33 Youden index (YI), and area under the curve (AUC) of 0.729 using age, family history, hypertension, waist circumference (WC), smoking, and alcohol consumption from 2001 and 2005 KNHANES data.
- Although cardiorespiratory fitness is related to risk factors for diabetes and is an important index for preventing and predicting diabetes [13,14], it has not been used in most prediction models for the risk of diabetes due to the associated difficulty and cost of its measurement. In contrast, resting heart rate (RHR) can be easily measured by anyone without any special equipment and is highly associated with obesity [15], stress [16], sympathetic nervous system [17], insulin [18], maximal oxygen comsumption [19,20], physical strength [21], and levels of physical activity [22]. Thus, RHR is a variable that could be used in risk prediction models for undiagnosed diabetes. In fact, a number of studies have demonstrated that high RHR is associated with the prevalence [23-28] and incidence of diabetes [29-31].
- Therefore, this study aimed to (1) determine whether the addition of RHR to an existing undiagnosed diabetes prediction model would improve predictability and validity, and (2) develop an undiagnosed diabetes prediction model using only RHR, age, and WC, and validates the predictability.
INTRODUCTION
- Study participants
- Data from 2010 to 2017 were used in this study [32]. A total of 40,059 participants over the age of 20, after excluding 5,769 with a missing family history of diabetes, 4,646 with missing smoking status, 4,699 with missing data for alcohol intake, 2,817 with missing WC, 5,931 with missing fasting blood glucose level, 2,606 with a missing diagnosis of diabetes, 1,936 who fasted less than 8 hours before blood sample collection, 2,889 with missing values for 60-second RHR, and one participant with RHR of 212 bpm, were analyzed. Data from 19,675 adults from 2010, 2012, 2014, and 2016 KNHANES were used to develop the model, and data from 19,917 adults from 2011, 2013, 2015, and 2017 KNHANES were used to validate the model (Figure 1). The general characteristics of the study participants are listed in Table 1.
- Measurement items and methods
- Height and weight were measured using a height meter (Seca 225; Seca, Hamburg, Germany) and scale (GL-6000-20; G-TECH, Seoul, Korea), respectively. WC was measured to one decimal place (0.1 cm) using a tape measure (Seca 200, Seca). The center of the lower end of the last rib and the upper end of the iliac crest on the participants’ side were measured [33].
- The RHR was measured as follows: The right arm radial pulse was measured for 15 seconds after completing a questionnaire in a sitting position and resting for more than 30 minutes. If the pulse was irregular, that is, bradycardia (less than 15 beats) or tachycardia (more than 26 beats), the pulse was measured for 60 seconds to assess the regularity of the pulse. The pulse rate for 60 seconds and the number of pulses for 15 seconds converted to 60 seconds were summed and analyzed [33].
- Participants with fasting blood glucose level greater than 126 mg/dL or glycated hemoglobin (HbA1c) greater than 6.5% (Figure 1) [34], but, have not been diagnosed with diabetes, or under no treatment for diabetes were considered to have undiagnosed diabetes.
- Lee et al. [12] developed a Korean undiagnosed diabetes risk prediction model based on age, family history of diabetes, hypertension, WC, smoking, and alcohol intake. The risk index of the model ranged from zero to 11.
- The RHR score added to the previously developed undiagnosed diabetes risk prediction model [12] consisted of odds ratio calculated by binary logistic regression analysis of RHR and undiagnosed diabetes. The RHR score was evaluated as follows: zero point for RHR < 60 bpm for men and < 65 bpm for women, one point for RHR of 60-89 bpm for men and 65-84 bpm for women, and two points for RHR of > 90 bpm for men and > 85 bpm for women. The risk index of the model ranged from zero to 13. Moreover, the model consisting of only three variables (RHR, age, and WC) had odds ratio calculated by binary logistic regression analysis of age, WC, and undiagnosed diabetes from KNHANES data of evennumbered years. Age < 40 years, 40-59 years, and > 60 years were given zero, four, and six points, respectively. The WC score was evaluated as follows: zero point for WC of < 84 cm for men and < 77 cm for women, two points for WC of 84-89 cm for men and 77-84 cm for women, and five points for WC of > 90 cm for men and > 85 cm for women. The risk index of the model ranged from zero to 13.
- Perkins & Schisterman [35] reported the optimized predictive diagnostic criterion using AUC as the minimum score of (1-sensitivity)2 +(1-specificity)2 or maximum score of YI (sensitivity+ specificity-1) [36]. The predictive diagnostic criteria for each model were: five points for the model by Lee et al. [12], seven points for total, women, and men for the model of current study, and seven points for total, seven points for men, and nine points for women for the model consisting of RHR, age, and WC.
- Statistical analysis
- Data were analyzed using the Statistical Package for the Social Sciences version 25.0 statistical program. Frequency analysis, crossanalysis, and independent sample t-tests were conducted for differences in demographic characteristics between men and women elderly individuals. Logistic regression analysis was conducted to estimate the prevalence of type 2 diabetes in the groups according to their RHR [37]. The AUC was also analyzed, and the validity of the model was compared by evaluating sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, negative likelihood ratio [38], YI (sensitivity+ specificity-1), and AUC [39]. Statistical significance was set at pvalue < 0.05.
- Ethics statement
- All procedures including study participants were approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (IRB No. 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C, 2013-07CON-03-4C, 2013-12EXP-03-5C, 2015-01-02-6C, 2018-01-03-P-A).
MATERIALS AND METHODS
Body composition test
Resting heart rate
Undiagnosed diabetes
Previously developed Korean undiagnosed diabetes risk prediction model
New Korean undiagnosed diabetes risk prediction model with addition of resting heart rate
Predictive diagnosis criteria
- Participants’ characteristics
- Participants’ characteristics according to gender are presented in Table 1. Compared to healthy participants (men: 68.40± 0.13 bpm; women: 70.40± 0.11 bpm), participants with undiagnosed diabetes (men: 71.36± 0.48 bpm; women: 71.63± 0.49 bpm) had significantly higher RHR (p < 0.001) and showed significantly higher body mass index, WC, blood glucose level, proportion of family history of diabetes, hypertension, daily alcohol intake, and lower income level.
- Association of resting heart rate, waist circumference and age with prevalence of undiagnosed diabetes
- Association of RHR, WC and age with prevalence of undiagnosed diabetes are presented in Table 2. The prevalence of undiagnosed diabetes was approximately 2.14-fold (95% confidence interval [CI], 1.53 to 2.97) higher in the group with the highest RHR than in the lowest RHR group. Additionally, the prevalence of undiagnosed diabetes was 6.68 (95% CI, 5.17 to 8.64) times higher in those over the age of 60 than in those under 40. The prevalence of undiagnosed diabetes was also 5.14 (95% CI, 4.26 to 6.21) times higher in the group with the highest WC than in the group with the lowest WC.
- Validity of the developed Korean undiagnosed diabetes risk prediction model
- Validity of the developed Korean undiagnosed diabetes risk prediction model are presented in Table 3. The Korean undiagnosed diabetes risk prediction model, which was previously developed using the results of the 2001 and 2005 KNHANES, was applied to the KNHANES data from even-numbered years (2010, 2012, 2014, and 2016). The sensitivity was 81% for men and 91% for women, and the specificity was 50% and 47% for men and women, respectively. ACU was 0.713 (95% CI, 0.689 to 0.736) and 0.773 (95% CI, 0.752 to 0.794) for men and women, respectively. The YI was 31 for men and 38 for women.
- The model was also applied to the KNHANES data from odd-numbered years. The sensitivity was 80% for men and 92% for women, and the specificity was 49% and 47% for men and women, respectively. AUC 0.703 (95% CI, 0.681 to 0.726) and 0.783 (95% CI, 0.763 to 0.802) for men and women, respectively. The YI was 29 for men and 39 for women.
- Validity of Korean undiagnosed diabetes risk prediction model with resting heart rate
- Validity of Korean undiagnosed diabetes risk prediction model with RHR are presented in Table 3. The RHR was added to the previously developed undiagnosed diabetes risk prediction model. The model was developed using data from the KNHANES in even-numbered years and validated using data from the KNHANES in odd-numbered years. The sensitivity was 66% for men and 82% for women, and the specificity was 65% and 64% for men and women, respectively. AUC was 0.711 (95% CI, 0.689 to 0.733) and 0.785 (95% CI, 0.766 to 0.804) for men and women, respectively. The YI was 31 for men and 46 for women. Compared to the previous model developed by Lee et al. [12], this new model with RHR had a 14% and 10% decrease in sensitivity for men and women, respectively. The specificity increased by 15% for men and 17% for women, and YI increased by two points for men and seven points for women.
- Validity of Korean undiagnosed diabetes risk prediction model consisting of resting heart rate, age, and waist circumference
- Validity of Korean undiagnosed diabetes risk prediction model consisting of RHR, age, and WC are presented in Table 3. A new undiagnosed diabetes risk prediction model was developed using RHR, age, and WC from KNHANES data in even-numbered years and validated using data from KNHANES in odd-numbered years. The sensitivity was 66% for men and 77% for women, and the specificity was 64% for men and 69% for women. AUC was 0.705 (95% CI, 0.683 to 0.727) and 0.786 (95% CI, 0.767 to 0.805) for men and women, respectively. YI was 30 points for men and 46 points for women. Compared to the previous model developed by Lee et al. [12], this new model consisting of only RHR, age, and WC had 14% and 15% decreases in sensitivity for men and women, respectively. The specificity increased by 15% for men and 22% for women, and YI was increased by one point for men and seven points for women.
RESULTS
- The main aim of the current study was to investigate whether adding RHR to the Korean diabetes risk prediction model developed in 2012 would affect the model’s predictability. Compared to the previous model [12], the specificity, YI, and AUC increased with the addition of RHR although it is not significant. Knowing that RHR is significantly associated with prevalence of undiagnosed diabetes, lack of significant improvement in prediction model when RHR was added is not because RHR is not an important factor. Rather, RHR was associated with variables used in the previous prediction model such as smoking [40], alcohol intake [41], and hypertension [42] and therefore RHR acts as a mediating or confounding factor in the undiagnosed diabetes risk model. One important observation worth reporting is that addition of RHR to existing prediction model reduced sensitivity but improved specificity of the model, in turn, YI or AUC is similar. When validation analyses were performed, Lee’s models [12] sensitivity was 86% and specificity was 49% while RHR was added to Lee’s model [12], sensitivity decreased to 74% but specificity increased to 65%. Since YI are similar between two model, we cannot say one is better than the other.
- The second aim of the current study was to develop and test model using only simple and easily accessible variabes including RHR, age, and WC would predict undiagnosed diabetes. Our results showed prediction model only used RHR were not inferior to previous developed model which used age, family history of diabetes, hypertentioin, WC, smoking, alcohol intake. This results further support discussion that RHR reflects one’s lifestyle factors such as such as smoking [40], alcohol intake [41], and hypertension [42] as previously mentioned. Therefore, the prediction model only used RHR, age, WC perform similar to Lee’s model [12] with RHR added.
- Furthermore, our data also showed participants with undiagnosed diabetes were younger than those diagnosed with diabetes, and men with undiagnosed diabetes had significantly higher fasting glucose levels than men with diagnosed diabetes. Taken together with previous studies [9] which showed delay in diabetes diagnosis resulted in late initation of treatment and increased risk of diabetes complication, our findings suggest the importance of early detection, initiation of treatment to control diabetes is of importance and potentially showed the usability of RHR in this process.
- Herein, a higher RHR was associated with the prevalence of undiagnosed diabetes. The group with the highest RHR was 2.14 times more likely to have undiagnosed diabetes than the group with the lowest RHR. Li et al. [43] analyzed the relationship between RHR and undiagnosed diabetes in 16,636 participants between the age of 35-78 and reported that men and women with RHR greater than 80 bpm had 3.66-times and 2.98-times higher prevalence of undiagnosed diabetes, respectively, than those with RHR less than 60 bpm. Althogh there are relatively fewer studies investigated association between RHR and undiagnosed diabetes, there are ample number of studies which reported that RHR is associated with revalence and also incidence of diabetes [23-31], suggesting that high RHR is associated with high blood glucose levels regardless of diagnosis of diabetes. Since RHR is associated with obesity [15], stress [16], sympathetic nervous system [17], insulin [18], maximal oxygen comsumption [19,20], physical strength [21], and levels of physical activity [22] and these factors are associated with insulin resistance and glucose metabolism, strong association between RHR and prevalence of diabetes is not surprising.
- Our results showed regardless of using Lee’s model [12], Lee’s model [12] plus RHR or model which only used RHR, age, and WC, model’s predictability was better in women than in men. In diabetes models of other countries, more points were allotted to men because men had higher prevalence of diabetes than women [10,11]. However, Lee’s model did not attribute additional points to men and this might have caused some gender differences in the performance of diabete prediction model. Since, the current study followed the same method as Lee’s model, we observed the similar gender difference as Lee’s model.
- Our data also showed awareness of diabetes is lower with younger age (46.0% for men and 56.9% for women in their 40s vs. 85.2% for men and 81.5% for women in their 60s), and only 7.0% of men and 5.6% of women in their 40s actively manage their blood glucose levels [44]. The recent advancements in information technology have allowed the creation of advanced medical devices software by combining wearable devices, artificial intelligence, and biomarkers. With advanced medical devices software, patients may prevent, manage, and treat diseases through digital therapeutics [45]. A randomized clinical study was conducted to verify the effectiveness of digital therapeutics in patients with hypertension [46]. Patienttailored analysis and precise medicine will be provided using data measured individually by the patients in the future. In particular, RHR and WC can be measured without special equipment and evaluated in real-time using wearable devices. Thus, it will help people with high diabetes risk to be aware of their risk of diabetes and encourange them to use medical services to manage their health.
- Several limitations must be considered when interpreting this study’s findings. Firstly, the KNHANES used to develop and validate the model was a cross-sectional study. The data may have been sufficient to investigate the prevalence of undiagnosed diabetes; however, it may be inadequate to study incidence of diabetes. Therefore, a diabetes risk prediction model must be developed using the incidence of diabetes from prospective cohort data. Secondly, since the oral glucose tolerance test was not performed for KNHANES, only fasting blood glucose and HbA1c were used for determination of undiagnosed diabetes. This may lead to an underestimation of patients with undiagnosed diabetes. Lastly, RHR may fluctuate depending on smoking, alcohol intake, sleep, and physical condition and therefore, caution must be exercised when single measure of RHR is used for risk prediction models.
- In conclusion, RHR is highly correlated with the prevalence of undiagnosed diabetes and could be used to increase the predictability of diabetes risk prediction models. Furthermore, the prediction model developed using only RHR, age and WC, which anyone can easily measure, had similar predictability to the previous diabetes risk prediction model. The results of this study may help develop future strategies or applications for predicting early undiagnosed diabetes.
DISCUSSION
SUPPLEMENTARY MATERIALS
-
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare for this study.
-
FUNDING
This study was funded by Yonsei Signature Research Cluster Program of 2021-22-0009.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Park DH, Jeon JY. Data curation: Park DH, Lee YH, Jee SH. Formal analysis: Park DH, Cho W. Funding acquisition: Jeon JY. Methodology: Cho W, Lee YH, Jee SH. Project administration: Jeon JY. Visualization: Park DH. Writing – original draft: Park DH, Jeon JY. Writing – review & editing: Park DH, Cho W, Lee YH, Jee SH, Jeon JY.
NOTES
ACKNOWLEDGEMENTS
| Characteristics |
Men |
p-value |
Women |
p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Non-diabetes (n=7,176) | Undiagnosed diabetes (n=385) | Diagnosed diabetes (n=767) | Non-diabetes (n=10,188) | Undiagnosed diabetes (n=355) | Diagnosed diabetes (n=804) | |||
| Age (yr) | 47.88±0.21 | 56.73±0.782,3 | 62.50±0.552 | <0.001 | 47.53±0.18 | 58.15±0.822,3 | 64.03±0.542 | <0.001 |
| Body mass index (kg/m2) | 24.11±0.04 | 25.65±0.172,3 | 24.70±0.122 | <0.001 | 23.14±0.04 | 26.45±0.182,3 | 25.19±0.122 | <0.001 |
| Waist circumference (cm) | 84.51±0.12 | 89.43±0.452 | 88.67±0.322 | <0.001 | 77.68±0.11 | 87.56±0.502,3 | 85.66±0.332 | <0.001 |
| RHR (bpm) | 68.40±0.13 | 71.36±0.482 | 70.61±0.342 | <0.001 | 70.40±0.11 | 71.63±0.492 | 71.73±0.332 | <0.001 |
| Fasting glucose (mg/dL) | 95.13±0.27 | 144.78±0.982,3 | 138.86±0.692 | <0.001 | 92.16±0.21 | 138.42±0.962 | 135.47±0.642 | <0.001 |
| HbA1c (%) | 5.53±0.01 | 7.10±0.032,3 | 7.29±0.022 | <0.001 | 5.51±0.01 | 7.12±0.032 | 7.26±0.022 | <0.001 |
| Family history of diabetes | 1,109 (15.5) | 80 (20.8) | 209 (27.2) | <0.001 | 1,781 (17.5) | 81 (22.8) | 226 (28.1) | <0.001 |
| Hypertension | 2,338 (32.6) | 230 (59.7) | 489 (63.8) | <0.001 | 2,412 (23.7) | 182 (51.3) | 549 (68.3) | <0.001 |
| Alcohol intake (drinks/day) | <0.001 | <0.001 | ||||||
| <1 | 4,680 (65.2) | 220 (57.1) | 509 (66.4) | 9,360 (91.9) | 336 (94.6) | 781 (97.1) | ||
| 1-5 | 2,022 (28.2) | 115 (29.9) | 193 (25.2) | 745 (7.3) | 17 (4.8) | 20 (2.5) | ||
| ≥5 | 474 (6.6) | 50 (13.0) | 65 (8.5) | 83 (0.8) | 2 (0.6) | 3 (0.4) | ||
| Smoking | <0.001 | 0.287 | ||||||
| Never | 1,586 (22.1) | 62 (16.1) | 99 (12.9) | 9,116 (89.5) | 326 (91.8) | 733 (91.2) | ||
| Past | 2,677 (37.3) | 177 (46.0) | 401 (52.3) | 549 (5.4) | 13 (3.7) | 33 (4.1) | ||
| Current | 2,913 (40.6) | 146 (37.9) | 267 (34.8) | 523 (5.1) | 16 (4.5) | 38 (4.7) | ||
| Education | <0.001 | <0.001 | ||||||
| Elementary | 1,665 (23.2) | 107 (27.8) | 194 (25.3) | 2,361 (23.2) | 106 (29.9) | 223 (27.7) | ||
| Middle school | 1,810 (25.2) | 100 (26.0) | 191 (24.9) | 2,530 (24.8) | 90 (25.4) | 205 (25.5) | ||
| High school | 1,832 (25.5) | 92 (23.9) | 177 (23.1) | 2,593 (25.5) | 83 (23.4) | 193 (24.0) | ||
| College | 1,829 (25.5) | 80 (20.8) | 200 (26.1) | 2,627 (25.8) | 74 (20.8) | 176 (21.9) | ||
| Income | 0.136 | 0.002 | ||||||
| Low | 913 (12.7) | 81 (21.0) | 189 (24.6) | 2,245 (22.0) | 156 (43.9) | 456 (56.7) | ||
| Middle low | 684 (9.5) | 54 (14.0) | 150 (19.6) | 966 (9.5) | 52 (14.6) | 118 (14.7) | ||
| Middle high | 2,544 (35.5) | 117 (30.4) | 231 (30.1) | 3,445 (33.8) | 96 (27.0) | 156 (19.4) | ||
| High | 2,895 (40.3) | 116 (30.1) | 179 (23.3) | 3,350 (32.9) | 42 (11.8) | 55 (6.8) | ||
Values are presented as mean±standard error or number (%).
RHR, resting heart rate; HbA1c, hemoglobin A1c; ANCOVA, analysis of covariance.
1 All variables were tested by ANCOVA or chi-square test; ANCOVA was performed with age as covariates.
2 p-value <0.05 vs. non-diabetes.
3 p-value <0.05 vs. diagnosed diabetes.
| Variables | Gender | Cut-off point | High risk (%) | Sensitivity (%) | Specificity (%) | PPV | NPV | PLR | NLR | Youden index | AUC (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Development set | ||||||||||||
| Lee1 | Total | 5 | 53 | 86 | 49 | 0.07 | 0.99 | 1.67 | 0.29 | 35 | 0.737 (0.721, 0.753) | |
| Men | 5 | 51 | 81 | 50 | 0.08 | 0.98 | 1.63 | 0.38 | 31 | 0.713 (0.689, 0.736) | ||
| Women | 5 | 54 | 91 | 47 | 0.06 | 0.99 | 1.73 | 0.19 | 38 | 0.773 (0.752, 0.794) | ||
| Lee1+RHR | Total | 7 | 36 | 73 | 65 | 0.08 | 0.98 | 2.09 | 0.42 | 38 | 0.748 (0.732, 0.763) | |
| Men | 7 | 47 | 77 | 55 | 0.08 | 0.98 | 1.72 | 0.41 | 32 | 0.719 (0.696, 0.742) | ||
| Women | 7 | 40 | 80 | 62 | 0.07 | 0.99 | 2.10 | 0.32 | 42 | 0.780 (0.760, 0.800) | ||
| Park2 | Total | 7 | 34 | 70 | 67 | 0.08 | 0.98 | 2.14 | 0.45 | 37 | 0.747 (0.732, 0.762) | |
| Men | 7 | 37 | 67 | 65 | 0.09 | 0.97 | 1.92 | 0.51 | 32 | 0.710 (0.687, 0.733) | ||
| Women | 7 | 32 | 73 | 69 | 0.08 | 0.99 | 2.36 | 0.39 | 42 | 0.778 (0.758, 0.798) | ||
| Validation set | ||||||||||||
| Lee1 | Total | 5 | 54 | 86 | 48 | 0.07 | 0.99 | 1.65 | 0.30 | 34 | 0.737 (0.722, 0.752) | |
| Men | 5 | 53 | 80 | 49 | 0.08 | 0.98 | 1.56 | 0.41 | 29 | 0.703 (0.681, 0.726) | ||
| Women | 5 | 54 | 92 | 47 | 0.06 | 0.99 | 1.74 | 0.18 | 39 | 0.783 (0.763, 0.802) | ||
| Lee+RHR | Total | 7 | 37 | 74 | 65 | 0.09 | 0.98 | 2.09 | 0.41 | 39 | 0.750 (0.731, 0.761) | |
| Men | 7 | 36 | 66 | 65 | 0.10 | 0.97 | 1.91 | 0.52 | 31 | 0.711 (0.689, 0.733) | ||
| Women | 7 | 37 | 82 | 64 | 0.08 | 0.99 | 2.30 | 0.28 | 46 | 0.785 (0.766, 0.804) | ||
| Park2 | Total | 7 | 35 | 71 | 67 | 0.09 | 0.98 | 2.14 | 0.43 | 38 | 0.749 (0.734, 0.763) | |
| Men | 7 | 38 | 66 | 64 | 0.10 | 0.97 | 1.84 | 0.53 | 30 | 0.705 (0.683, 0.727) | ||
| Women | 7 | 33 | 77 | 69 | 0.09 | 0.99 | 2.46 | 0.33 | 46 | 0.786 (0.767, 0.805) | ||
Cut-off point, highest Youden index; PPV, positive predictive value; NPV, negative predictive value, PLR, positive likelihood ratio; NLR, negative likelihood ratio; AUC, area under the curve; RHR, resting heart rate; WC, waist circumference.
Korean undiagnosed diabetes screen score (Lee model [16]): (35 years≤age≤44 years)*2+(age ≥45 years)*3+(family history of diabetes)*1+(hypertension)*1+[men: (84 cm≤WC≤89.9 cm), women: (77 cm≤WC≤83.9 cm)]*2+[men: (WC ≥90 cm), women: (WC ≥84 cm)]*3+(current smoker)*1+(1≤drinks/day≤4.9)*1+(drinks/day ≥5)*2.
1 Lee model+RHR: [men: (60 bpm≤RHR≤74 bpm), women: (65 bpm≤RHR≤74 bpm)]*1+[men: (75 bpm≤RHR≤89 bpm), women: (75 bpm≤RHR≤84 bpm)]*1+[men: (RHR ≥90 bpm), women: (RHR ≥85 bpm)]*2.
2 Park model: (40 years≤age≤59 years)*4+(age ≥60 years)*6+[men: (60 bpm≤RHR≤74 bpm), women: (65 bpm≤RHR≤74 bpm)]*1+[men: (75 bpm≤RHR≤89 bpm), women: (75 bpm≤RHR≤84 bpm)]*1+[men: (RHR ≥90 bpm), women: (RHR ≥85 bpm)]*2+[men: (84 cm≤WC≤89.9 cm), women: (77 cm≤WC≤84 cm)]*2+[men: (WC ≥90 cm), women: (WC ≥85 cm)]*5.
- 1. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J 2021;45:1-10.ArticlePubMedPMCPDF
- 2. Statistics Korea. Cause of death; 2018 [cited 2020 Feb 28]. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E02&conn_path=I2 (Korean).
- 3. Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1 · 9 million people. Lancet Diabetes Endocrinol 2015;3:105-113.ArticlePubMedPMC
- 4. Ergul A, Kelly-Cobbs A, Abdalla M, Fagan SC. Cerebrovascular complications of diabetes: focus on stroke. Endocr Metab Immune Disord Drug Targets 2012;12:148-158.ArticlePubMedPMC
- 5. Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: epidemiology, mechanisms, and outcomes. World J Diabetes 2015;6:961-969.ArticlePubMedPMC
- 6. Cusick M, Meleth AD, Agrón E, Fisher MR, Reed GF, Knatterud GL, et al. Associations of mortality and diabetes complications in patients with type 1 and type 2 diabetes: early treatment diabetic retinopathy study report no. 27. Diabetes Care 2005;28:617-625.PubMed
- 7. Young BA, Lin E, Von Korff M, Simon G, Ciechanowski P, Ludman EJ, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care 2008;14:15-23.PubMedPMC
- 8. Centers for Disease Control and Prevention. National diabetes statistics report; 2020 [cited 2020 Sep 1]. Available from: https://www.cdc.gov/diabetes/library/features/diabetes-stat-report.html.
- 9. Lee YH, Armstrong EJ, Kim G, Oh J, Kang SM, Lee BW, et al. Undiagnosed diabetes is prevalent in younger adults and associated with a higher risk cardiometabolic profile compared to diagnosed diabetes. Am Heart J 2015;170:760-769.ArticlePubMed
- 10. Bang H, Edwards AM, Bomback AS, Ballantyne CM, Brillon D, Callahan MA, et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med 2009;151:775-783.ArticlePubMedPMC
- 11. Griffin SJ, Little PS, Hales CN, Kinmonth AL, Wareham NJ. Diabetes risk score: towards earlier detection of type 2 diabetes in general practice. Diabetes Metab Res Rev 2000;16:164-171.ArticlePubMed
- 12. Lee YH, Bang H, Kim HC, Kim HM, Park SW, Kim DJ. A simple screening score for diabetes for the Korean population: development, validation, and comparison with other scores. Diabetes Care 2012;35:1723-1730.PubMedPMC
- 13. Carnethon MR, Sternfeld B, Schreiner PJ, Jacobs DR Jr, Lewis CE, Liu K, et al. Association of 20-year changes in cardiorespiratory fitness with incident type 2 diabetes: the coronary artery risk development in young adults (CARDIA) fitness study. Diabetes Care 2009;32:1284-1288.PubMedPMC
- 14. Zaccardi F, O’Donovan G, Webb DR, Yates T, Kurl S, Khunti K, et al. Cardiorespiratory fitness and risk of type 2 diabetes mellitus: a 23-year cohort study and a meta-analysis of prospective studies. Atherosclerosis 2015;243:131-137.ArticlePubMed
- 15. Zhang SY, Wu JH, Zhou JW, Liang Z, Qiu QY, Xu T, et al. Overweight, resting heart rate, and prediabetes/diabetes: a populationbased prospective cohort study among Inner Mongolians in China. Sci Rep 2016;6:23939.ArticlePubMedPMCPDF
- 16. Shalev AY, Sahar T, Freedman S, Peri T, Glick N, Brandes D, et al. A prospective study of heart rate response following trauma and the subsequent development of posttraumatic stress disorder. Arch Gen Psychiatry 1998;55:553-559.ArticlePubMed
- 17. Grassi G, Vailati S, Bertinieri G, Seravalle G, Stella ML, Dell’Oro R, et al. Heart rate as marker of sympathetic activity. J Hypertens 1998;16:1635-1639.ArticlePubMed
- 18. Anderson EA, Hoffman RP, Balon TW, Sinkey CA, Mark AL. Hyperinsulinemia produces both sympathetic neural activation and vasodilation in normal humans. J Clin Invest 1991;87:2246-2252.ArticlePubMedPMC
- 19. Gonzales TI, Jeon JY, Lindsay T, Westgate K, Perez-Pozuelo I, Hollidge S, et al. Resting heart rate as a biomarker for tracking change in cardiorespiratory fitness of UK adults: the Fenland Study. medRxiv [Preprint] 2020;[cited 2020 Feb 28]. Available from: https://doi.org/10.1101/2020.07.01.20144154.Article
- 20. Nauman J, Aspenes ST, Nilsen TI, Vatten LJ, Wisløff U. A prospective population study of resting heart rate and peak oxygen uptake (the HUNT Study, Norway). PLoS One 2012;7:e45021.ArticlePubMedPMC
- 21. Silva DA, de Lima TR, Tremblay MS. Association between resting heart rate and health-related physical fitness in Brazilian adolescents. Biomed Res Int 2018;2018:3812197.ArticlePubMedPMCPDF
- 22. Emaus A, Degerstrøm J, Wilsgaard T, Hansen BH, Dieli-Conwright CM, Furberg AS, et al. Does a variation in self-reported physical activity reflect variation in objectively measured physical activity, resting heart rate, and physical fitness? Results from the Tromso study. Scand J Public Health 2010;38(5 Suppl):105-118.ArticlePubMedPDF
- 23. Yang HI, Kim HC, Jeon JY. The association of resting heart rate with diabetes, hypertension, and metabolic syndrome in the Korean adult population: the fifth Korea National Health and Nutrition Examination Survey. Clin Chim Acta 2016;455:195-200.ArticlePubMed
- 24. Kim DI, Yang HI, Park JH, Lee MK, Kang DW, Chae JS, et al. The association between resting heart rate and type 2 diabetes and hypertension in Korean adults. Heart 2016;102:1757-1762.ArticlePubMed
- 25. Park H, Lee J, Kim JY, Kim DI, Jeon JY. The relationship between resting heart rate and prevalence of metabolic syndrome and type 2 diabetes mellitus in Korean adults: the fifth Korea National Health and Nutrition Examination Survey (2012). Korean J Obes 2015;24:166-174 (Korean).Article
- 26. Cho W, Kim DI, Min JH, Jeon JY. The association of resting heart rate and muscular endurance and prevalence with type 2 diabetes in Korean adults. Exerc Sci 2017;26:259-266 (Korean).ArticlePDF
- 27. Hong JW, Noh JH, Kim DJ. The association of resting heart rate with the presence of diabetes in Korean adults: the 2010-2013 Korea National Health and Nutrition Examination Survey. PLoS One 2016;11:e0168527.ArticlePubMedPMC
- 28. Park DH, Hong SH, Cho W, Jeon JY. Higher resting heart rate and lower relative grip strength is associated with increased risk of diabetes in Korean elderly population: Korean National Health and Nutrition Examination Survey 2015-2018. Exerc Sci 2020;29:416-426 (Korean).ArticlePDF
- 29. Lee DH, de Rezende LF, Hu FB, Jeon JY, Giovannucci EL. Resting heart rate and risk of type 2 diabetes: a prospective cohort study and meta-analysis. Diabetes Metab Res Rev 2019;35:e3095.ArticlePubMedPMCPDF
- 30. Kim G, Lee YH, Jeon JY, Bang H, Lee BW, Kang ES, et al. Increase in resting heart rate over 2 years predicts incidence of diabetes: a 10-year prospective study. Diabetes Metab 2017;43:25-32.ArticlePubMed
- 31. Aune D, Ó Hartaigh B, Vatten LJ. Resting heart rate and the risk of type 2 diabetes: a systematic review and dose--response metaanalysis of cohort studies. Nutr Metab Cardiovasc Dis 2015;25:526-534.ArticlePubMed
- 32. Korea Disease Control and Prevention Agency. Examine survey guideline; 2018 [cited 2020 Feb 28]. Available from: https://knhanes.kdca.go.kr/knhanes/sub04/sub04_02_02.do?classType=4 (Korean).
- 33. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 2014;43:69-77.ArticlePubMedPMC
- 34. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care 2019;42(Suppl 1):S13-S28.ArticlePubMedPDF
- 35. Perkins NJ, Schisterman EF. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol 2006;163:670-675.ArticlePubMedPMC
- 36. Youden WJ. Index for rating diagnostic tests. Cancer 1950;3:32-35.ArticlePubMed
- 37. Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression. Hoboken: Wiley; 2013. p 47-54.
- 38. Brenner H, Gefeller O. Variation of sensitivity, specificity, likelihood ratios and predictive values with disease prevalence. Stat Med 1997;16:981-991.ArticlePubMed
- 39. Bradley AP. The use of the area under the ROC curve in the evaluation of machine learning algorithms. Pattern Recognit 1997;30:1145-1159.Article
- 40. Linneberg A, Jacobsen RK, Skaaby T, Taylor AE, Fluharty ME, Jeppesen JL, et al. Effect of smoking on blood pressure and resting heart rate: a mendelian randomization meta-analysis in the CARTA consortium. Circ Cardiovasc Genet 2015;8:832-841.ArticlePubMedPMC
- 41. Conrod PJ, Peterson JB, Pihl RO, Mankowski S. Biphasic effects of alcohol on heart rate are influenced by alcoholic family history and rate of alcohol ingestion. Alcohol Clin Exp Res 1997;21:140-149.ArticlePubMed
- 42. Shi Y, Zhou W, Liu X, Ping Z, Li YQ, Wang C, et al. Resting heart rate and the risk of hypertension and heart failure: a dose-response meta-analysis of prospective studies. J Hypertens 2018;36:995-1004.PubMed
- 43. Li YQ, Sun CQ, Li LL, Wang L, Guo YR, You AG, et al. Resting heart rate as a marker for identifying the risk of undiagnosed type 2 diabetes mellitus: a cross-sectional survey. BMC Public Health 2014;14:1052.ArticlePubMedPMCPDF
- 44. Korean Diabetes Association. Diabetes fact sheet in Korea 2016; 2018 [cited 2021 Feb 9]. Available from: https://www.diabetes.or.kr/temp/KDA_fact_sheet%202016.pdf (Korean).
- 45. Kim HS, Kwon IH, Cha WC. Future and development direction of digital healthcare. Healthc Inform Res 2021;27:95-101.ArticlePubMedPMCPDF
- 46. Kario K, Nomura A, Kato A, Harada N, Tanigawa T, So R, et al. Digital therapeutics for essential hypertension using a smartphone application: a randomized, open-label, multicenter pilot study. J Clin Hypertens (Greenwich) 2021;23:923-934.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

- Comparisons of the prediction models for undiagnosed diabetes between machine learning versus traditional statistical methods
Seong Gyu Choi, Minsuk Oh, Dong–Hyuk Park, Byeongchan Lee, Yong-ho Lee, Sun Ha Jee, Justin Y. Jeon
Scientific Reports.2023;[Epub] CrossRef - Factors related to undiagnosed diabetes in Korean adults: a secondary data analysis
Bohyun Kim
Journal of Korean Biological Nursing Science.2023; 25(4): 295. CrossRef
- Figure
- Related articles
-
- Development and validation of the Health Literacy Index for the Community (HLIC) for the Korean National Health and Nutrition and Examination Survey
- Association of healthy lifestyle factors with the risk of hypertension, dyslipidemia, and their comorbidity in Korea: results from the Korea National Health and Nutrition Examination Survey 2019-2021
- Mediating effect of lower extremity muscle on the relationship between obesity and osteoarthritis in middle-aged and elderly women in Korea: based on the 2009-2011 Korea National Health and Nutrition Examination Survey
- Associations of the magnesium depletion score and magnesium intake with diabetes among US adults: an analysis of the National Health and Nutrition Examination Survey 2011-2018
- Folate, vitamin B12, and homocysteine status in the Korean population: data from the 2013-2015 Korea National Health and Nutrition Examination Survey

 KSE
KSE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite


