Abstract
-
OBJECTIVES
- We conducted a comorbidity network analysis using data from the seventh Korea National Health and Nutrition Examination Survey to systematically quantify obesity-related comorbidities.
-
METHODS
- The study included 11,712 subjects aged 45 to 80 (5,075 male and 6,637 female). A prevalent disease was defined as a specific disease for which a subject had been diagnosed by a doctor and was being treated. Comorbidity network analysis was performed for diseases with a prevalence of 1% or more, including overweight and obesity. We estimated the observed-to-expected ratio of all possible disease pairs with comorbidity strength and visualized the network of obesity-related comorbidities.
-
RESULTS
- In subjects over 45 years old, 37.3% of people had a body mass index over 25.0 kg/m2. The most common prevalent disease was hypertension (42.3%), followed by dyslipidemia (17.4%) and diabetes (17.0%). Overweight and obese subjects were 2.1 times (95% confidence interval, 1.9 to 2.3) more likely to have a comorbidity (i.e., 2 or more diseases) than normal-weight subjects. Metabolic diseases such as hypertension, dyslipidemia, diabetes, and osteoarthritis were directly associated with overweight and obesity. The probability of coexistence for each of those 4 diseases was 1.3 times higher than expected. In addition, hypertension and dyslipidemia frequently coexisted in overweight and obese female along with other diseases. In obese male, dyslipidemia and diabetes were the major diseases in the comorbidity network.
-
CONCLUSIONS
- Our results provide evidence justifying the management of metabolic components in obese individuals. In addition, our results will help prioritize interventions for comorbidity reduction as a public health goal.
-
Keywords: Comorbidity, Multimorbidity, Obesity, Network analysis
INTRODUCTION
- According to a World Health Organization report, 39% of adults over the age of 18 worldwide had a body mass index (BMI) of 25.0 kg/m2 or higher in 2016 [1]. This trend has increasing steadily over the past 3 decades [2], and a similar trend has been observed in Korea [3]. The high prevalence of obesity is a public health challenge. In 2017, the Global Burden of Disease project reported that high BMI accounted for 4 million deaths globally and also contributed to 120 million disability-adjusted life-years [4]. As normal weight maintenance and weight loss are associated with many health benefits, obesity prevention and management are among the top public health priorities. Moreover, the global prevalence of overweight and obesity among children and adolescents aged 5 to 19 increased from 4% in 1975 to 18% in 2016 [1]. Due to this trend, the burden of obesity is expected to continue.
- It is well-known that obesity is a major risk factor for chronic diseases such as cardiovascular disease (CVD), some type of cancers, and metabolic diseases [5]. While obesity is clearly linked to a variety of diseases, there continue to be questions about how many obesity-related diseases exist and how closely they relate to each other. The relationship between various diseases and obesity is not straightforward and can be difficult to explain. For example, the effect of obesity on CVD could be explained by other mediating metabolic diseases. Although some studies have shown relationships between obesity and various diseases [6,7], few have quantified these relationships overall. In order to quantify these relationships, we conducted a comorbidity network analysis. Network analysis is a methodological approach for the systematic evaluation of complex relationships [8] that can help illuminate the natural progression of chronic diseases. Studies on diabetes and hypertension have reported results of comorbidity network analyses based on claims data [9,10]. Since obesity is not classified as a clinical disease, it is only possible to grasp the relationship between obesity and other diseases using large-scale survey data, rather than administrative data. Therefore, in this study, we systematically analyzed comorbidity patterns related to obesity through network analysis using data from the Korea National Health and Nutrition Examination Survey (KNHANES).
MATERIALS AND METHODS
- Data
- For this study, we used data from the seventh KNHANES (2016- 2018). The KNHANES is a nationally representative survey that is conducted annually to assess health-related behaviors, chronic disease conditions, and trends in food and nutrition intake. The KNHANES consists of 3 component surveys: a health interview, a health examination, and a nutrition survey. A sampling plan was conducted before every wave of the survey (every 3 years) and relied on a multi-stage sampling method. The detailed KNHANES survey method has been published elsewhere [11]. The seventh survey collected data from 2016 to 2018, with a response rate of 76.6%. It collected data on 24,269 people between 1 year and 80 years old (8,150 in 2016, 8,127 in 2017, and 7,992 in 2018). Since the prevalence of chronic diseases increases with age, we only included middle-aged and elderly subjects (45-80 years old, n= 12,193). After the exclusion of subjects with missing data regarding disease-related questions and BMI, 11,712 subjects were ultimately included in the study (5,075 male and 6,637 female).
- Overweight and obesity definition and assessment of prevalent diseases
- A person with a BMI equal to or more than 25.0 kg/m2 was considered overweight/obese. Overweight and obesity were determined based on BMI, which was calculated using data from measurements of subjects’ height and weight. Although the criterion for overweight in Asian countries is lower than that in Western countries, this study used the criterion of 25.0 kg/m2 as a general standard to define overweight. Thirty diseases were investigated using data from the seventh KNHANES survey of chronic disease conditions. They were hypertension, dyslipidemia, stroke, coronary artery disease (myocardial infarction or angina), osteoarthritis, rheumatoid arthritis, osteoporosis arthritis, tuberculosis, asthma, diabetes, thyroid disease, stomach cancer, liver cancer, colorectal cancer, breast cancer, cervical cancer, lung cancer, thyroid cancer, depression, atopic dermatitis, allergic rhinitis, sinusitis, otitis media, cataract, glaucoma, macular degeneration, kidney failure, hepatitis B, hepatitis C, and cirrhosis. A prevalent disease was defined as a specific disease in a subject that had been diagnosed by a doctor and was being treated at the time of the survey. Hypertension and diabetes specifically were determined using blood pressure and fasting blood glucose data according to the criteria reported by the Korea Centers for Disease Control and Prevention [12,13]. These variable units were labeled 0 (no) and 1 (yes).
- Comorbidity network analysis
- The research goal of the comorbidity network was to assess whether diseases tend to appear together more frequently than expected. The basic elements of network analysis consist of nodes and edges. Nodes indicate specific diseases, and edges indicate the coexistence of a pair of diseases. Due to the nature of the study design, the edges between diseases have no directionality. To identify obesity-related comorbidities, we considered overweight and obesity (BMI≥ 25.0 kg/m2) as a node. For comorbidity strength, we estimated the observed-to-expected ratio (OER) of all possible disease pairs based on previous studies of comorbidity networks [14]. The numerator of the OER is the observed coexistence scale of a disease pair, and the denominator is the expected coexistence scale of a disease pair under the assumption of independence. Thus, the OER can be expressed as follows:
- Where a is the proportion with coexistence of diseases i and j; b is the prevalence of disease i; c is the prevalence of disease j.
- Statistical tests were performed on the proportional differences between the denominator and the numerator, and p-values were calculated with continuity correction. For disease pairs with pvalue< 0.05 and OER> 1.0, the relationship was visualized using visNetwork, an R package for network visualization. The diameter of each node represents the prevalence of each disease, and the thickness of edges represents the OER value. Network clustering was analyzed using the “infomap” algorithm of the igraph R package [15]. Thus, the same clusters are represented by nodes of the same color in our visualizations. We estimated the strength, degree, closeness, and betweenness of diseases (nodes) in the network to determine their relative importance. The strength is determined by the sum of the strength of all the connections of a specific disease. Degree is measured by the number of direct connections to a disease. Closeness is a quantified relationship that includes indirect connections from a specific disease in the network. High closeness, for example, indicates a short average distance between a specific disease and all other diseases. Betweenness measures the importance of nodes in the average pathway between other pairs of diseases [8]. For every pair of diseases in a connected graph, there is at least 1 shortest path between diseases. The betweenness of each disease is defined as the number of these shortest paths going through a disease. Diseases present in less than 1% of the total population were not included in the network analysis. We performed an initial comorbidity network analysis including all subjects, followed by analyses of people considered obese of each sex. A sensitivity analysis was performed with overweight and obesity defined using a BMI threshold of 23.0 kg/m2 or higher.
- Statistical analysis
- For summary statistics, the results for continuous variables were presented as weighted means with standard error (SE), while those for categorical variables were presented as the number of subjects with weighted percentages based on multi-stage sampling. The 30 diseases were listed according to the prevalence rate, and diseases with a prevalence rate of 1% or more were tabulated. The risk of having a prevalent disease according to sex or obesity was evaluated using logistic regression and results were expressed as an odds ratio (OR) with a 95% confidence interval (CI). Statistical significance was assessed at p-value < 0.05 with a 2-tailed test. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) or R version 3.6.2 (https://cran.rproject.org/bin/windows/base/old/3.6.2/).
- Ethics statement
- There was no personal information included in the KNHANES data, and ethical approval for the use of open KNHANES data was exempted from the Institutional Review Board (IRB) Committee of the Ewha Womans University Hospital (IRB No. EUMC 2020-08-007).
RESULTS
- Of subjects over 45 years old, 37.33% (SE, 0.56) had a BMI that exceeded 25 kg/m2. Of that percentage, female accounted for 49.16% (SE, 0.88). It was reported that 70.43% (SE, 0.84) of obese subjects had at least 1 of the 30 prevalent diseases, and 40.16% (SE 0.86) had 2 or more prevalent diseases. In non-obese subjects, 56.38% (SE, 0.75) of subjects had 1 prevalent disease, and 26.63% (SE, 0.65) had 2 or more prevalent diseases (Table 1).
- The associations between high BMI (≥ 25.0 kg/m2) and having a disease with a prevalence rate of more than 1% are presented in Table 2. The most common disease was hypertension (42.28%), followed by dyslipidemia (17.43%) and diabetes (17.04%). Those with overweight and obesity had a 2.34 times (95% CI, 2.12 to 2.58) higher risk of hypertension than those who are not obese. Overweight and obesity were also associated with prevalent diseases such as dyslipidemia, diabetes, osteoarthritis, thyroid disease, stroke, and coronary artery disease. The high-BMI group had a 2.08 times (95% CI, 1.89 to 2.29) higher risk of comorbid disease than their low-BMI counterparts when adjusted for sex and age.
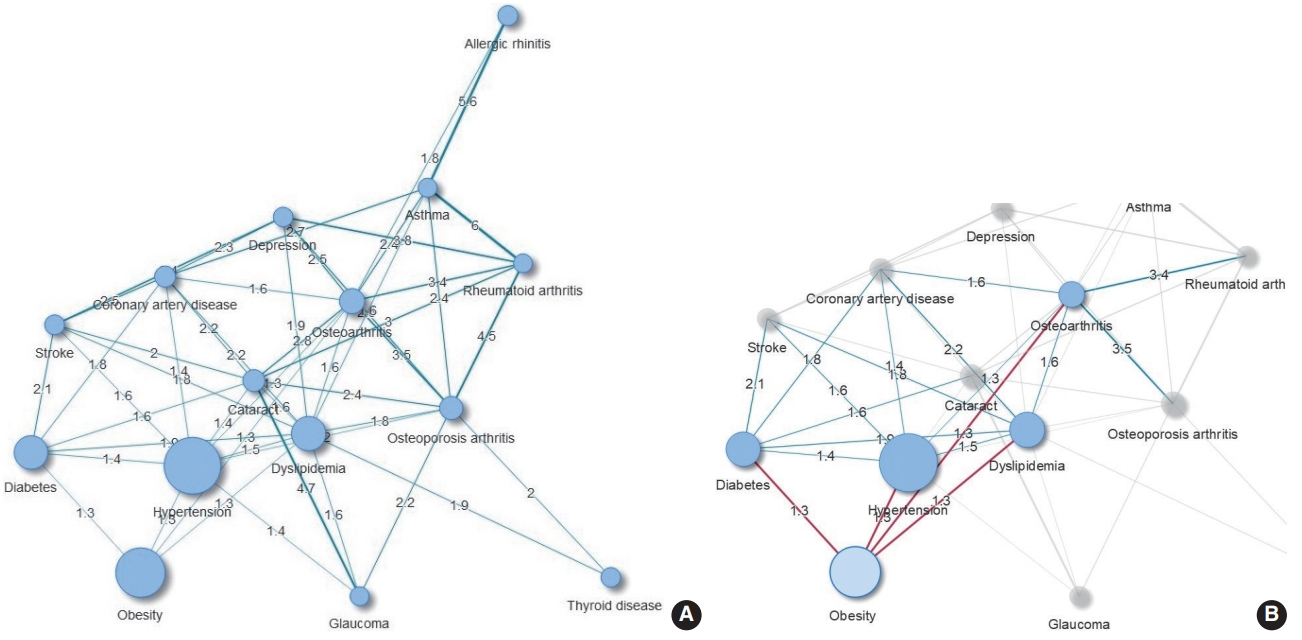
- The results of the comorbidity network analysis related to obesity are shown in Figure 1. One cluster was identified (Figure 1A). The number of subjects with obesity who also had hypertension, diabetes, dyslipidemia, or osteoarthritis was 30% higher than expected. Additionally, obesity was indirectly associated with CVDs through metabolic diseases (hypertension, diabetes, and dyslipidemia). Cataracts were linked to obesity through diabetes (Figure 1B). The results were also consistent when defining overweight and obesity as having a BMI of 23.0 kg/m2 or higher (data not shown).
- We also evaluated the rates of prevalent diseases in obese subjects by sex (Table 3). Dyslipidemia and musculoskeletal diseases were more common in females than in males. Cataracts, thyroid disease, and depression were also more frequent in females than in males. However, hypertension, diabetes, and coronary artery disease were more common in males than in females. In overweight and obese subjects, the comorbidity risk was higher in females than in males by 1.22 times (95% CI, 1.05 to 1.42) after the results were adjusted for age.
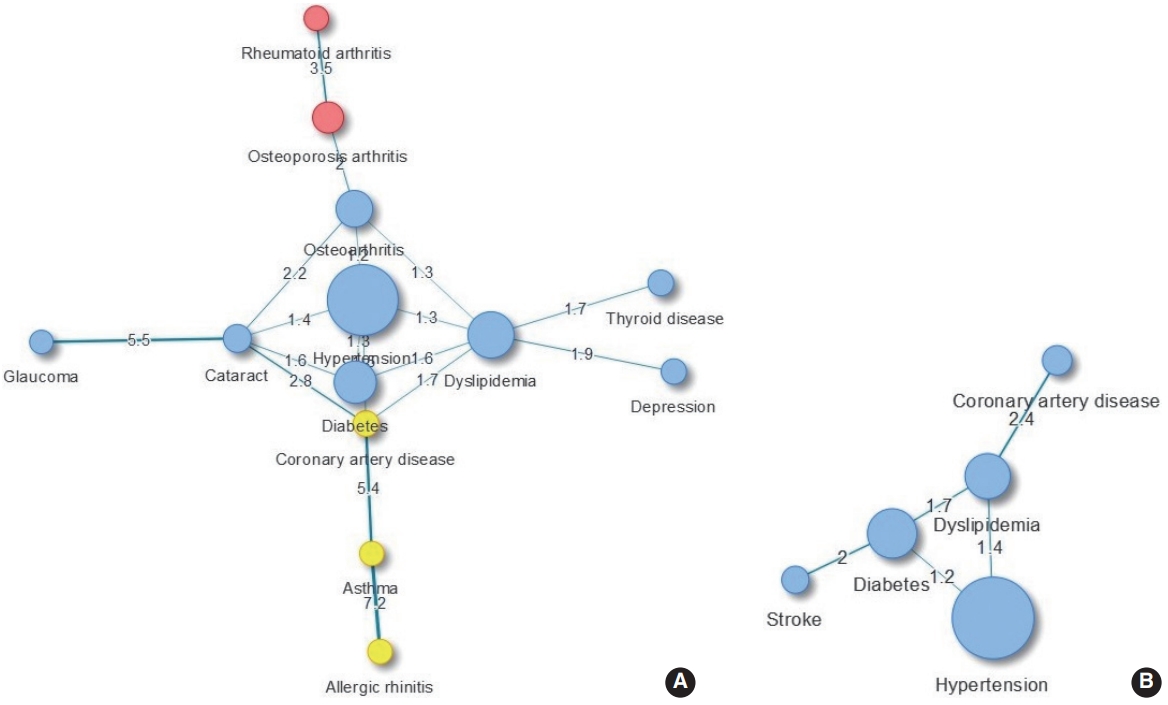
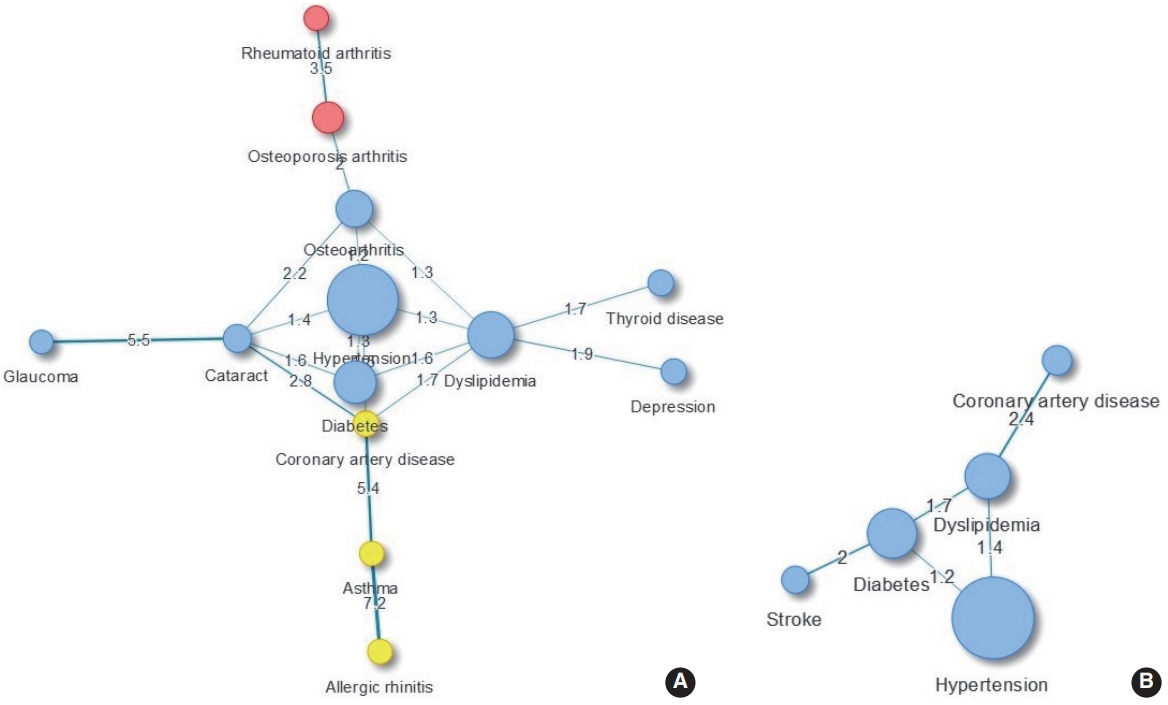
- We evaluated the major comorbidities of obese subjects by sex using network analysis. In females, 3 clusters were identified: (1) metabolic diseases, thyroid disease, depression, and ophthalmic diseases were classified into one cluster; (2) musculoskeletal diseases; (3) otorhinolaryngologic and coronary artery diseases. Diseases such as thyroid disease and depression were shown to accompany dyslipidemia, and the proportion of diabetes and cataract comorbidities was 1.64 times as high as expected (95% CI, 1.09 to 2.47) (Figure 2A). In obese males, the proportion of dyslipidemia and coronary artery disease comorbidities, which appeared as a cluster, was more than 2.4 times higher than expected, and the proportion of diabetes and stroke comorbidities was 2 times higher than expected (Figure 2B). When the comorbidity network was analyzed for betweenness, hypertension and dyslipidemia were the major diseases in obese females, and dyslipidemia and diabetes were the major diseases in obese males. These tendencies remained unchanged even when an analysis based on closeness was conducted (Table 4).
DISCUSSION
- Through comorbidity network analysis, we identified the major obesity-related comorbid diseases using large-scale survey data. Metabolic diseases such as hypertension, dyslipidemia, diabetes, and osteoarthritis were directly associated with overweight and obesity, and the comorbidity risk in overweight and obesity subjects was 2.1 times higher than in normal-weight subjects. Furthermore, in overweight and obese people, dyslipidemia, hypertension, and diabetes were frequently accompanied by other diseases, and were characterized as close to other diseases. Moreover, based on their betweenness, we found that these metabolic diseases play a central role in mediating between diseases in the network. Therefore, managing metabolic components and weight loss reduces the likelihood of developing BMI-related diseases and comorbidities.
- Although obesity has been accepted as a predisposing factor for the development of various chronic diseases such as CVD and metabolic diseases, the definition of obesity-related diseases has unclear boundaries. Comorbidity network analysis provides insights to help understand obesity-related diseases and can provide information for patient care and treatment in a medical setting [9,10,16]. By obtaining data on the prevalence of chronic diseases with a long disease duration, a snapshot was taken of the distribution of comorbid diseases, and our results are in line with those of previous studies. Some paired diseases had a higher prevalence than expected in terms of the OER. This finding means that these diseases do not have an independent distribution, but instead are closely related to other conditions.
- The relationship between metabolic diseases and high BMI is well established based on accumulated evidence [5,7]. Large-scale survey studies in the United States and Europe have reported that hypertension, dyslipidemia, and diabetes are linked to overweight and obesity in a dose-dependent manner [17,18]. Among the 4 diseases directly related to overweight and obesity, metabolic diseases are frequently accompanied by other diseases, and CVD, which is significantly related to obesity, appears to have a relationship to these diseases. A pathway mediated by metabolic diseases in the relationship between obesity and CVD has also been suggested in previous studies [5,19]. Coronary artery disease has been shown to accompany dyslipidemia in both obese males and females, and was 2.4 times and 1.7 times more frequent than expected, respectively. The coexistences of asthma and coronary artery disease was significant in obese females. According to a metaanalysis, an association between asthma and coronary artery disease was predominantly found in females [20]. In addition, obesity had a high likelihood of being accompanied by hypertension, diabetes, and dyslipidemia (p-value for all pairs < 0.01) (Figure 2), which may increase the risk of subsequent disease. Indeed, a study found that the prevalence of coronary artery disease was often more than doubled among patients with concomitant conditions with hypertension and dyslipidemia compared to those with only 1 condition [21]. Therefore, it is important for clinicians to understand and manage comorbid diseases in order to prevent diseases that increase patients’ risk of disability and premature death.
- The prevalence of musculoskeletal diseases was higher in obese females than in obese males, and the coexistence of osteoarthritis and hypertension was also found to be significant in obese females, which aligns with the results of previous studies [22-24]. The relationship between osteoarthritis and hypertension remains controversial, but it has been proposed that obesity may be involved as a pathomechanism [25]. Musculoskeletal diseases are known to impair functional parameters such as mobility, subsequently reducing quality of life [26]. A comorbidity study showed that those with osteoarthritis reported a low quality of life regardless of the type of comorbid disease [23]. A quantitative systematic review evaluated the effect of weight loss on osteoarthritis symptoms and reported that weight loss in obese patients diagnosed with knee arthritis appeared to improve physical disability and pain levels [27]. Since the likelihood of musculoskeletal diseases increases with age, efforts to improve quality of life are needed along with treatment and management.
- Among endocrine diseases, thyroid disease was significantly associated with overweight and obesity. Although the types of thyroid diseases associated with overweight and obesity have not been investigated in detail, a study in Korea showed that hypothyroidism has a higher prevalence than hyperthyroidism [28]. Of these diseases, hypothyroidism is more closely related to obesity, and it may also affect lipid profiles [29]. In an UpToDate review, it was reported that patients with hypercholesterolemia should be screened for hypothyroidism before lipid-lowering therapy [30]. However, since thyroid disease is underdiagnosed, the accuracy of the assessment of the coexistence of thyroid disease with other diseases seems to be low. Among other endocrine diseases, diabetes commonly coexisted with hypertension or dyslipidemia, but it also coexisted frequently with cataracts. These results are consistent with those of a previous study [10]. The coexistence of diabetes and cataracts and the coexistence of thyroid disease and dyslipidemia were more prevalent in obese females than in obese males. On the contrary, the coexistence of stroke and diabetes was frequent in obese males, but not in obese females. It seems that there were meaningful differences in the prevalence of these conditions between male and female. Sex differences in the prevalence of comorbidities have been studied elsewhere and help to account for differences in life expectancy between male and female [18,31].
- There were several points to keep in mind when interpreting the results. Our results were derived from a cross-sectional survey, so an analysis of causality is not appropriate. Some uncertainty by measurement error and self-reported disease information may have influenced the results. The data source used did not include patients with severe conditions who had been hospitalized, which would have affected prevalence estimates. Our study utilized measured BMI information, but the diseases that could be considered were limited according to the scope of the survey data. Although a positive association between obesity and non-alcoholic fatty liver disease (NAFLD) has been reported [5], NAFLD is not covered in the KNHANES. Using a limited range of survey data inevitably limited the scope of our evaluation. While we used 3-year combined data, the data used for our analysis were utilized on a small scale according to the conditions of interest. Therefore, we were limited in our ability to subdivide subjects into separate overweight and obese groups. In addition, since significance was determined according to the size of the dataset, the significance level was not controlled for multiple comparisons.
- Nevertheless, results were obtained using data representing the Korean population, so there are benefits to the generalized scope of the results. By using survey data rather than administrative data, our study provides information on obesity-related comorbidities through a systematic approach. Its findings can motivate the public to manage and prevent, as well as better understand, overweight and obesity. Finally, through network analysis, we systematically evaluated obesity-related diseases and provided insights for further research. The study can also provide helpful information for prioritizing interventions for comorbidity reduction as a public health measure.
- In summary, taking into account the possibility of modification, preventing overweight and obesity through weight loss is expected to reduce the risk and severity of various chronic diseases. Furthermore, managing metabolic components in obese persons reduces the chance of developing comorbid diseases.
NOTES
-
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare for this study.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: HAL. Data curation: HAL. Formal analysis: HAL. Funding acquisition: None. Methodology: HAL, HP. Project administration: HAL. Visualization: HAL. Writing – original draft: HAL. Writing – review & editing: HAL, HP.
ACKNOWLEDGEMENTS
None.
Figure 1.Comorbidity network in adults over 45 years of age (A) and obesity-related comorbidities (B) (n=11,712). Node size is proportional to the prevalence of the corresponding comorbidity. Same-colored nodes indicate the same cluster. Edge thickness indicates the observed-to-expected ratio value for connected conditions.

Figure 2.Comorbidity network in obese female (A) and obese male (B) over 45 years of age. Node size is proportional to the prevalence of the corresponding comorbidity. Same-colored nodes indicate the same cluster. Edge thickness indicates the observed-to-expected ratio value for connected conditions.
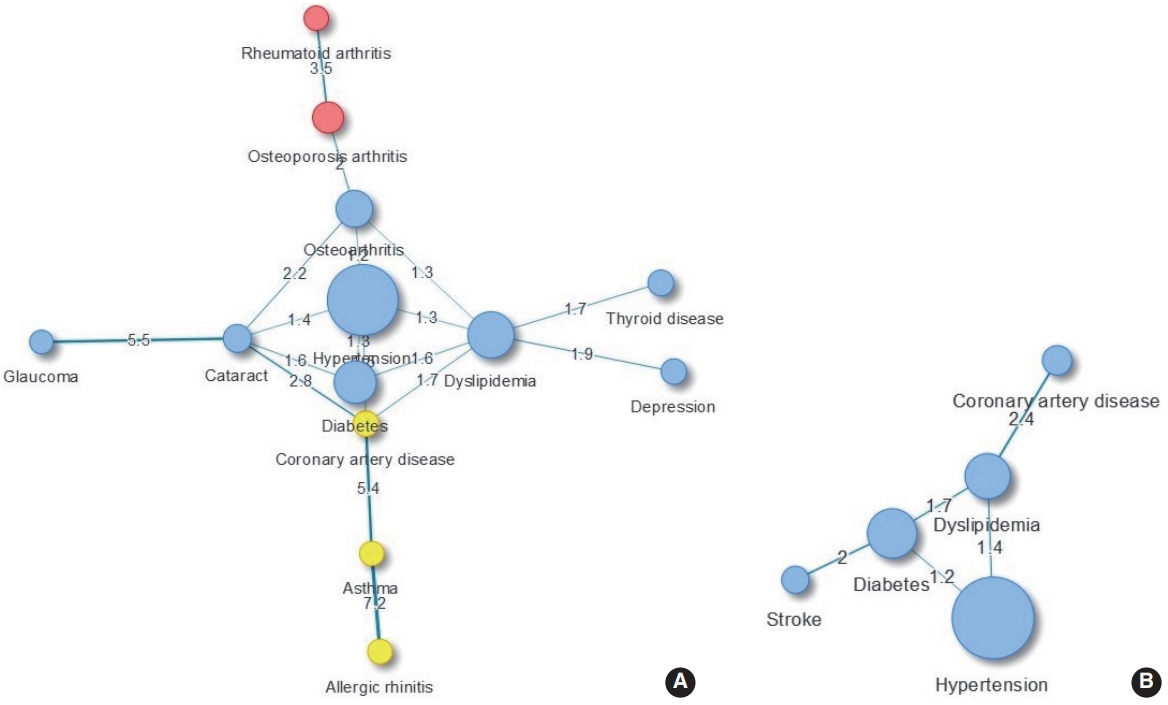
Table 1.Basic characteristics of study subjects
|
Characteristics |
BMI <25.0 kg/m2 (n=7,356) |
BMI ≥25.0 kg/m2 (n=4,356) |
|
Age (yr) |
59.73 [0.18] |
59.60 [0.22] |
|
Sex, male |
3,111 (45.94)/[0.59] |
1,964 (50.84)/[0.88] |
|
BMI (kg/m2) |
22.29 [0.03] |
27.44 [0.04] |
|
No. of comorbidities among 30 prevalent diseases |
|
0 |
2,889 (43.62)/[0.75] |
1,111 (29.57)/[0.84] |
|
1 |
2,187 (29.75)/[0.64] |
1,293 (30.28)/[0.79] |
|
2 |
1,328 (15.86)/[0.49] |
1,034 (22.33)/[0.75] |
|
3 |
610 (7.15)/[0.35] |
562 (11.11)/[0.50] |
|
4 |
235 (2.50)/[0.20] |
246 (4.74)/[0.37] |
|
≥5 |
107 (1.11)/[0.13] |
110 (1.98)/[0.22] |
Table 2.Diseases with a prevalence of more than 1% in adults over 45 years of age and differences according to high BMI (n=11,712)1
|
Ranking of prevalent diseases |
Total (n=11,712) |
BMI, kg/m2
|
|
<25.0 (n=7,356) |
≥25.0 (n=4,356) |
≥25.0 vs. <25.02
|
|
1. Hypertension |
5,362 (42.28) |
2,861 (35.41) |
2,501 (53.83) |
2.34 (2.12, 2.58) |
|
2. Dyslipidemia |
2,274 (17.43) |
1,182 (14.22) |
1,092 (22.81) |
1.84 (1.65, 2.06) |
|
3. Diabetes |
2,173 (17.04) |
1,115 (13.78) |
1,058 (22.51) |
1.87 (1.68, 2.08) |
|
4. Osteoarthritis |
1020 (7.20) |
529 (5.91) |
491 (9.36) |
1.69 (1.44, 1.99) |
|
5. Osteoporosis arthritis |
760 (5.26) |
505 (5.45) |
255 (4.93) |
0.83 (0.69, 1.01) |
|
6. Cataracts |
573 (3.89) |
370 (4.10) |
203 (3.54) |
0.84 (0.68, 1.04) |
|
7. Coronary artery disease |
444 (3.09) |
249 (2.74) |
195 (3.68) |
1.44 (1.16, 1.79) |
|
8. Allergic rhinitis |
325 (2.90) |
211 (3.02) |
114 (2.69) |
0.90 (0.68, 1.18) |
|
9. Stroke |
301 (2.26) |
176 (2.04) |
125 (2.63) |
1.35 (1.01, 1.79) |
|
10. Thyroid |
266 (2.17) |
154 (1.96) |
112 (2.52) |
1.41 (1.04, 1.90) |
|
11. Depression |
255 (1.86) |
152 (1.77) |
103 (2.01) |
1.15 (0.86, 1.54) |
|
12. Asthma |
175 (1.31) |
105 (1.26) |
70 (1.38) |
1.10 (0.78, 1.57) |
|
13. Glaucoma |
181 (1.29) |
111 (1.20) |
70 (1.43) |
1.23 (0.87, 1.74) |
|
14. Rheumatoid arthritis |
157 (1.17) |
93 (1.20) |
64 (1.11) |
0.93 (0.64, 1.36) |
|
Comorbidity (2 or more diseases)3
|
4,232 (31.68) |
2,280 (26.63) |
1,952 (40.16) |
2.08 (1.89, 2.29) |
Table 3.Diseases with a prevalence of more than 1% in overweight and obese adults over 45 years of age by sex1
|
Ranking of prevalent diseases |
Total (n=4,356) |
Male (n=1,964, 45.1%) |
Female (n=2,392, 54.9%) |
Female vs. male2
|
|
1. Hypertension |
2,501 (53.83) |
1,123 (54.13) |
1,378 (53.52) |
0.70 (0.60, 0.81) |
|
2. Dyslipidemia |
1,092 (22.81) |
414 (19.20) |
678 (26.55) |
1.26 (1.07, 1.49) |
|
3. Diabetes |
1,058 (22.51) |
494 (22.34) |
564 (22.69) |
0.81 (0.69, 0.97) |
|
4. Osteoarthritis |
491 (9.36) |
85 (3.51) |
406 (15.41) |
3.87 (2.90, 5.18) |
|
5. Osteoporosis arthritis |
255 (4.93) |
9 (0.38) |
246 (9.63) |
20.05 (9.04, 44.45) |
|
6. Cataracts |
203 (3.54) |
48 (1.67) |
155 (5.48) |
2.03 (1.37, 3.01) |
|
7. Coronary artery disease |
195 (3.68) |
107 (4.21) |
88 (3.12) |
0.47 (0.34, 0.66) |
|
8. Allergic rhinitis |
114 (2.69) |
54 (2.74) |
60 (2.63) |
1.09 (0.70, 1.68) |
|
9. Stroke |
125 (2.63) |
63 (2.67) |
62 (2.58) |
0.71 (0.46, 1.09) |
|
10. Thyroid |
112 (2.52) |
17 (1.04) |
95 (4.04) |
4.49 (2.46, 8.18) |
|
11. Depression |
103 (2.01) |
18 (0.79) |
85 (3.28) |
3.77 (2.07, 6.87) |
|
12. Glaucoma |
70 (1.43) |
39 (1.91) |
31 (0.93) |
0.36 (0.21, 0.60) |
|
13. Asthma |
70 (1.38) |
20 (0.89) |
50 (1.89) |
1.32 (0.66, 2.63) |
|
14. Rheumatoid arthritis |
64 (1.11) |
5 (0.16) |
59 (2.09) |
10.71 (3.95, 29.02) |
|
Comorbidity (2 or more diseases)3
|
1,952 (40.16) |
757 (34.16) |
1,195 (46.36) |
1.22 (1.05, 1.42) |
Table 4.Results of evaluating the centrality of nodes in the comorbidity network of overweight and obesity in sexes over 45 years of age
|
Diseases |
Overweight and obesity
|
Female
|
Male
|
|
Strength |
Degree |
Closeness |
Betweenness |
Strength |
Degree |
Closeness |
Betweenness |
|
Diabetes |
4.50 |
3 |
0.20 |
0 |
4.84 |
3 |
0.45 |
3 |
|
Thyroid disease |
1.71 |
1 |
0.17 |
0 |
- |
- |
- |
- |
|
Depression |
1.91 |
1 |
0.16 |
0 |
- |
- |
- |
- |
|
Cataracts |
13.46 |
5 |
0.20 |
11 |
- |
- |
- |
- |
|
Glaucoma |
5.48 |
1 |
0.10 |
0 |
- |
- |
- |
- |
|
Asthma |
12.61 |
2 |
0.11 |
11 |
- |
- |
- |
- |
|
Allergic rhinitis |
7.18 |
1 |
0.06 |
0 |
- |
- |
- |
- |
|
Osteoarthritis |
6.66 |
4 |
0.22 |
20 |
- |
- |
- |
- |
|
Rheumatoid arthritis |
3.46 |
1 |
0.11 |
0 |
- |
- |
- |
- |
|
Osteoporosis arthritis |
5.45 |
2 |
0.17 |
11 |
- |
- |
- |
- |
|
Hypertension |
6.64 |
5 |
0.24 |
21 |
2.62 |
2 |
0.42 |
0 |
|
Dyslipidemia |
9.49 |
6 |
0.23 |
21 |
5.45 |
3 |
0.44 |
3 |
|
Stroke |
- |
- |
- |
- |
1.96 |
1 |
0.27 |
0 |
|
Coronary artery disease |
11.43 |
4 |
0.21 |
20 |
2.39 |
1 |
0.25 |
0 |
REFERENCES
- 1. World Health Organization. Obesity and overweight; 2020 [cited 2020 Jul 6]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 2. Institute for Health Metrics and Evaluation. Overweight and obesity Viz. [cited 2020 Jul 7]. Available from: https://vizhub.healthdata.org/obesity/.
- 3. Statistics Korea. Prevalence of obesity. [cited 2020 Jul 2]. Available from: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=2705 (Korean).Article
- 4. GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13-27.ArticlePubMedPMC
- 5. Pi-Sunyer X. The medical risks of obesity. Postgrad Med 2009;121:21-33.ArticlePubMedPMC
- 6. Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010;67:220-229.ArticlePubMed
- 7. Lee HA, Park H. Diet-related risk factors for incident hypertension during an 11-year follow-up: the Korean Genome Epidemiology Study. Nutrients 2018;10:1077.ArticlePubMedPMC
- 8. Hevey D. Network analysis: a brief overview and tutorial. Health Psychol Behav Med 2018;6:301-328.ArticlePubMedPMC
- 9. Liu J, Ma J, Wang J, Zeng DD, Song H, Wang L, et al. Comorbidity analysis according to sex and age in hypertension patients in China. Int J Med Sci 2016;13:99-107.ArticlePubMedPMC
- 10. Khan A, Uddin S, Srinivasan U. Comorbidity network for chronic disease: a novel approach to understand type 2 diabetes progression. Int J Med Inform 2018;115:1-9.ArticlePubMed
- 11. Khan A, Uddin S, Srinivasan U. Comorbidity network for chronic disease: a novel approach to understand type 2 diabetes progression. Int J Med Inform 2018;115:1-9.ArticlePubMed
- 12. Shin JY. Trends in the prevalence and management of diabetes in Korea: 2007-2017. Epidemiol Health 2019;41:e2019029.ArticlePubMedPMC
- 13. Kim HC, Ihm SH, Kim GH, Kim JH, Kim KI, Lee HY, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology of hypertension. Clin Hypertens 2019;25:16.ArticlePubMedPMC
- 14. Fotouhi B, Momeni N, Riolo MA, Buckeridge DL. Statistical methods for constructing disease comorbidity networks from longitudinal inpatient data. Appl Netw Sci 2018;3:46.ArticlePubMedPMC
- 15. Csardi G, Nepusz T. The igraph software package for complex network research. Inter J Complex Syst 2006;1695:1695.
- 16. Aguado A, Moratalla-Navarro F, López-Simarro F, Moreno V. MorbiNet: multimorbidity networks in adult general population. Analysis of type 2 diabetes mellitus comorbidity. Sci Rep 2020;10:2416.ArticlePubMedPMC
- 17. Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg 2008;207:928-934.ArticlePubMed
- 18. Peytremann-Bridevaux I, Santos-Eggimann B. Health correlates of overweight and obesity in adults aged 50 years and over: results from the Survey of Health, Ageing and Retirement in Europe (SHARE). Obesity and health in Europeans aged > or = 50 years. Swiss Med Wkly 2008;138:261-266.PubMed
- 19. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects), Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1· 8 million participants. Lancet 2014;383:970-983.ArticlePubMedPMC
- 20. Wang L, Gao S, Yu M, Sheng Z, Tan W. Association of asthma with coronary heart disease: a meta analysis of 11 trials. PLoS One 2017;12:e0179335.ArticlePubMedPMC
- 21. Johnson ML, Pietz K, Battleman DS, Beyth RJ. Prevalence of comorbid hypertension and dyslipidemia and associated cardiovascular disease. Am J Manag Care 2004;10:926-932.PubMed
- 22. Singh G, Miller JD, Lee FH, Pettitt D, Russell MW. Prevalence of cardiovascular disease risk factors among US adults with self-reported osteoarthritis: data from the Third National Health and Nutrition Examination Survey. Am J Manag Care 2002;8(15 Suppl):S383-S391.PubMed
- 23. Park B, Ock M, Lee HA, Lee S, Han H, Jo MW, et al. Multimorbidity and health-related quality of life in Koreans aged 50 or older using KNHANES 2013-2014. Health Qual Life Outcomes 2018;16:186.ArticlePubMedPMC
- 24. Marshall DA, Liu X, Barnabe C, Yee K, Faris PD, Barber C, et al. Existing comorbidities in people with osteoarthritis: a retrospective analysis of a population-based cohort in Alberta, Canada. BMJ Open 2019;9:e033334.ArticlePubMedPMC
- 25. Zhang YM, Wang J, Liu XG. Association between hypertension and risk of knee osteoarthritis: a meta-analysis of observational studies. Medicine (Baltimore) 2017;96:e7584.PubMedPMC
- 26. Shapses SA, Pop LC, Wang Y. Obesity is a concern for bone health with aging. Nutr Res 2017;39:1-13.ArticlePubMedPMC
- 27. Christensen R, Bartels EM, Astrup A, Bliddal H. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 2007;66:433-439.ArticlePubMedPMC
- 28. Kwon H, Jung JH, Han KD, Park YG, Cho JH, Lee DY, et al. Prevalence and annual incidence of thyroid disease in Korea from 2006 to 2015: a nationwide population-based cohort study. Endocrinol Metab (Seoul) 2018;33:260-267.ArticlePubMedPMC
- 29. Sanyal D, Raychaudhuri M. Hypothyroidism and obesity: an intriguing link. Indian J Endocrinol Metab 2016;20:554-557.ArticlePubMedPMC
- 30. Ross DS. Lipid abnormalities in thyroid disease; 2014 [cited 2020 Jul 14]. Available from: https://www.uptodate.com/contents/lipid-abnormalities-in-thyroid-disease.
- 31. Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, Poblador-Plou B, Calderón-Meza JM, Sicras-Mainar A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr 2014;14:75.ArticlePubMedPMC
Citations
Citations to this article as recorded by

- Metabolically healthy obese individuals are still at high risk for diabetes: Application of the marginal structural model
Hye Ah Lee, Hyesook Park
Diabetes, Obesity and Metabolism.2024; 26(2): 431. CrossRef - Comorbidity Patterns in Older Patients Undergoing Hip Fracture Surgery: A Comorbidity Network Analysis Study
Chiyoung Lee, Sijia Wei, Eleanor S. McConnell, Hideyo Tsumura, Tingzhong (Michelle) Xue, Wei Pan
Clinical Nursing Research.2024; 33(1): 70. CrossRef - Interaction between depressive symptoms and obesity-related anthropometric measures on multimorbidity among community-dwelling older adults: evidence from India
Waquar Ahmed, T. Muhammad, CV Irshad
BMC Public Health.2024;[Epub] CrossRef - Chronic disease and multimorbidity in the Chinese older adults’ population and their impact on daily living ability: a cross-sectional study of the Chinese Longitudinal Healthy Longevity Survey (CLHLS)
Ye Chen, Huixia Ji, Yang Shen, Dandan Liu
Archives of Public Health.2024;[Epub] CrossRef - Comorbidity increases the risk of pulmonary tuberculosis: a nested case-control study using multi-source big data
Bao-Yu Wang, Ke Song, Hai-Tao Wang, Shan-Shan Wang, Wen-Jing Wang, Zhen-Wei Li, Wan-Yu Du, Fu-Zhong Xue, Lin Zhao, Wu-Chun Cao
BMC Pulmonary Medicine.2024;[Epub] CrossRef - Charting paths to recovery: Navigating traumatic brain injury comorbidities through graph theory–exploring benefits and challenges
Shyam Kumar Sudhakar, Kaustav Mehta
Brain Organoid and Systems Neuroscience Journal.2024; 2: 10. CrossRef - Trends in prevalence of multimorbidity for chronic diseases in China: serial cross-sectional surveys from 2009 to 2018
Wei-Quan Lin, Li-Ying Luo, Yao-Hui Li, Min-Ying Sun, Qin Zhou, Yun-Ou Yang, Xiang-Yi Liu, Jia-Min Chen, Hui Liu
The Journal of nutrition, health and aging.2024; 28(8): 100260. CrossRef - Changes in Clinical Manifestations Due to AFLD Retyping Based on the New MAFLD Criteria: An Observational Study Based on the National Inpatient Sample Database
Xiaoshan Feng, Ruirui Xuan, Yingchun Dong, Xiaoqin Wu, Yiping Cheng, Zinuo Yuan, Hang Dong, Junming Han, Fang Zhong, Jiajun Zhao, Xiude Fan
Diagnostics.2023; 13(3): 488. CrossRef - The impact of obesity: a narrative review
BenjaminChih Chiang Lam, AmandaYuan Ling Lim, SooLing Chan, MabelPo Shan Yum, NatalieSi Ya Koh, EricAndrew Finkelstein
Singapore Medical Journal.2023; 64(3): 163. CrossRef - Prevalence of comorbidities post mild traumatic brain injuries: a traumatic brain injury model systems study
Shyam Kumar Sudhakar, Shreya Sridhar, Satvika Char, Kathan Pandya, Kaustav Mehta
Frontiers in Human Neuroscience.2023;[Epub] CrossRef - BMI trajectories, associations with outcomes and predictors in elderly gastric cancer patients undergoing radical gastrectomy: a prospective longitudinal observation study
Yinning Guo, Yimeng Chen, Xueyi Miao, Jieman Hu, Kang Zhao, Lingyu Ding, Li Chen, Ting Xu, Xiaoman Jiang, Hanfei Zhu, Xinyi Xu, Qin Xu
Journal of Cancer Survivorship.2023;[Epub] CrossRef - Factors associated with the combination of general and abdominal obesity in middle-aged and older Korean women: a cross-sectional study
Jin Suk Ra
Osong Public Health and Research Perspectives.2023; 14(5): 379. CrossRef - Progression and trajectory network of age-related functional impairments and their combined associations with mortality
Hui Chen, Binghan Wang, Rongxia Lv, Tianjing Zhou, Jie Shen, Huan Song, Xiaolin Xu, Yuan Ma, Changzheng Yuan
iScience.2023; 26(12): 108368. CrossRef - Body-mass index and risk of obesity-related complex multimorbidity: an observational multicohort study
Mika Kivimäki, Timo Strandberg, Jaana Pentti, Solja T Nyberg, Philipp Frank, Markus Jokela, Jenni Ervasti, Sakari B Suominen, Jussi Vahtera, Pyry N Sipilä, Joni V Lindbohm, Jane E Ferrie
The Lancet Diabetes & Endocrinology.2022; 10(4): 253. CrossRef - A national survey on current clinical practice pattern of Korean Medicine doctors for treating obesity
Kyung Hwan Jegal, Mi Mi Ko, Bo-Young Kim, Mi Ju Son, Sungha Kim, Alessandro de Sire
PLOS ONE.2022; 17(3): e0266034. CrossRef - Multimorbidity and combined interventions for patients with coronary heart disease in Chinese population: Latent class analysis of a multi-center study
Yuanyuan Chen, Junru Wu, Yan Tang, Zhengxin Li, Qing Wen, Xuejing Sun, Hong Yuan, Yao Lu, Jingjing Cai
International Journal of Cardiology.2022; 368: 17. CrossRef - Multimorbidity patterns by health-related quality of life status in older adults: an association rules and network analysis utilizing the Korea National Health and Nutrition Examination Survey
Thi-Ngoc Tran, Sanghee Lee, Chang-Mo Oh, Hyunsoon Cho
Epidemiology and Health.2022; 44: e2022113. CrossRef
 , Hyesook Park2,3
, Hyesook Park2,3



 KSE
KSE

 PubReader
PubReader ePub Link
ePub Link Cite
Cite