Articles
- Page Path
- HOME > Epidemiol Health > Volume 41; 2019 > Article
-
Review
Impact of pharmacist-led home medicines review services on drug-related problems among the elderly population: a systematic review -
Sai Krishna Gudi1
 , Ananth Kashyap2
, Ananth Kashyap2 , Manik Chhabra3
, Manik Chhabra3 , Muhammed Rashid4
, Muhammed Rashid4 , Komal Krishna Tiwari5
, Komal Krishna Tiwari5 -
Epidemiol Health 2019;41:e2019020.
DOI: https://doi.org/10.4178/epih.e2019020
Published online: May 17, 2019
1Rady Faculty of Health Sciences, University of Manitoba College of Pharmacy, Winnipeg, Canada
2Department of Pharmacy Practice, Sarada Vilas College of Pharmacy, Mysuru, India
3Department of Pharmacy Practice, Indo-Soviet Friendship College of Pharmacy, Moga, India
4Department of Pharmacy Practice, Sri Adichunchanagiri College of Pharmacy, Adichunchanagiri University, Bala Gangadharanatha Nagara, Karnataka, India
5Department of Physiotherapy and Rehabilitation Sciences, Jagadguru Sri Shivarathreeshwara, College of Physiotherapy, Rajiv Gandhi University of Health Sciences, Karnataka, India
- Correspondence: Sai Krishna Gudi Rady Faculty of Health Sciences, University of Manitoba College of Pharmacy, 750 McDermot Ave W, Winnipeg, MB R3E 0T5, Canada E-mail: sknanu06@gmail.com
©2019, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
- To address and elucidate the impact of pharmacist-led home medicines review (HMR) services on identifying drug-related problems (DRPs) among the elderly population in home care settings.
-
METHODS
- A comprehensive systematic search was performed using electronic scientific databases such as PubMed, Scopus, Embase, and Web of Science for studies published between January 1, 2008 and December 31, 2018, pertaining to HMR services by pharmacists for identifying DRPs.
-
RESULTS
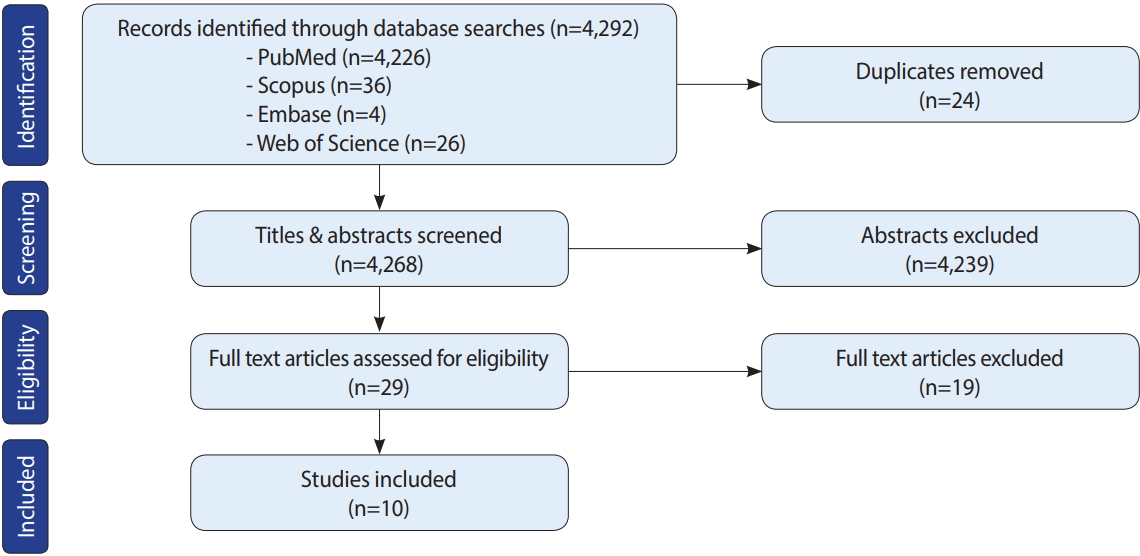
- In total, 4,292 studies were retrieved from the searches, of which 24 were excluded as duplicates. Titles and abstracts were screened for the remaining 4,268 studies, of which 4,239 were excluded due to the extraneous nature of the titles and/or abstracts. Subsequently, 29 full-text articles were assessed, and 19 were removed for lacking the outcome of interest and/or not satisfying the study’s inclusion criteria. Finally, 10 studies were included in the review; however, publication bias was not assessed, which is a limitation of this study. In all studies, pharmacists identified a highly significant amount of DRPs through HMR services. The most common types of DRPs were potential drug-drug interactions, serious adverse drug reactions, need for an additional drug, inappropriate medication use, non-adherence, untreated indications, excessive doses, and usage of expired medications.
-
CONCLUSIONS
- HMR is a novel extended role played by pharmacists. The efficiency of such programs in identifying and resolving DRPs could minimize patients’ health-related costs and burden, thereby enhancing the quality of life and well-being among the elderly.
- In countries with numerous and diverse populations, chronic diseases such as hypertension, diabetes, arthritis, and heart disease are common, especially among geriatric individuals; as a result, polypharmacy is a frequently occurring phenomenon in the elderly. Polypharmacy may give rise to various drug-related problems (DRPs), such as drug-drug interactions, adverse drug reactions (ADRs), medication errors, and drug-food interactions, which could eventually reduce levels of medication adherence [1]. At times, elderly patients might not take their medications as prescribed, which could evolve into altering the dose, frequency, or terminating the medication itself. The reasons for this may vary from simple logistical misunderstandings of factors such as the appropriate timing and dosage to a deeper misunderstanding of the purpose of a medication. Thus, inappropriate medication use among this vulnerable population is a major health concern [2]. ADRs are a major burden to patients, as shown by the fact that they are considered the fifth most common cause of death amongst hospitalized patients, with a notable morbidity rate of 5.6% in India. Therefore, several studies have been conducted to develop strategies for minimizing and preventing DRPs, including home medicines review (HMR) programs [3,4].
- In 2001, the Australian government initiated the first HMR program, defined as a consumer-focused, structured, and collaborative health care service in the community setting to promote better medication adherence [5]. It is a team-based approach that involves a clinician, pharmacist, and consumer to optimize the quality use of medicines and to improve consumers’ understanding of their medications. HMR starts with a referral by a clinician, which enables the pharmacist to visit the patient’s home in order to review the current medication therapy of that particular patient, to check for potential DRPs, and to resolve them in consultation with the responsible clinician [1,2]. The essential goal of the HMR program is to reduce the DRPs that are derived from inappropriate use of medicines, as doing so could enhance patients’ medication adherence [6]. In this review, we sought to critically inspect studies of the effects of pharmacist-initiated HMR programs on identifying and mitigating DRPs.
INTRODUCTION
- Data sources and search strategy
- A comprehensive search was performed of PubMed, Scopus, Embase, and Web of Science for peer-reviewed, full-text articles published in the English language between January 1, 2008 and December 31, 2018. Relevant keywords such as “HMR,” “home medicines review,” “drug related problems,” “pharmacist,” and “elderly” were searched in diverse combinations with Medical Subject Headings (MeSH) terms by using Boolean operators to identify all relevant studies. The detailed search strategy interpretation using PubMed was as follows: (“HMR” [All Fields] OR “home medicines review” [All Fields]) AND “drug-related problems” [All Fields] AND “pharmacists” [MeSH Terms] OR “pharmacists” [All Fields] AND (“aged” [MeSH Terms] OR “aged” [All Fields] OR “elderly” [All Fields]) AND (“2008/01/01” [PDAT]: “2018/12/31” [PDAT]). Any further missing publications were searched by checking the references of the included studies. ProQuest, Google Scholar, and Open Grey were searched for the grey literature.
- Study selection and data extraction
- Three reviewers (SKG, AK, and MC) independently screened the title and abstract of each article, and the potentially eligible full-texts of relevant abstracts were obtained and screened to identify articles of interest based on the study’s inclusion criteria, which were studies (prospective, retrospective, cross-sectional, or randomized) evaluating the impact of pharmacist-led HMR services on identifying DRPs among the elderly population. Articles were excluded if the outcome data were not reported in enough detail, the participants were not elderly, and the studies were conducted elsewhere from home or home care facilities; additionally, duplicate publications, literature reviews, conference abstracts, studies with no pharmacist involvement, and editorials/letters to the editor were excluded. The retrieved studies were imported into the Rayyan software [7] to remove duplicates and to review studies based on the inclusion and exclusion criteria. From each included study, the following data were extracted: author name(s), publication year, country, study design, sample size, mean age of the participants, key findings, and the summary. Any disagreements amongst the researchers regarding the inclusion of the studies were resolved through consensus, and a priori protocol was developed, and can be found in the Supplementary Material 1.
- Risk of bias and quality assessment
- The risk of bias and methodological quality of each included study were assessed by 2 independent reviewers (AK and SKG) using the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields [8], a 14-item measurement tool used to assess the methodological quality of the studies in a systematic review. Each item/question was scored as 2 (if the response was ‘yes’), 1 (if the response was ‘partial’), or 0 (if the response was ‘no’). Questions that were not applicable to a particular study were marked as ‘n/a’ and were excluded from the calculation of the summary score, which was calculated for each paper by summing the total score obtained for all items and dividing it by the total possible score. A higher summary score indicated a lower risk of bias and better study quality. Disagreements were resolved by discussions or by a third reviewer.
- Outcome assessment
- The outcome of interest of this review was DRPs, which were assessed in terms of their frequency, type, and nature as described in each included study. DRPs were defined as an event or circumstance involving drug therapy that potentially interfered with desired health outcomes.
MATERIALS AND METHODS
- Initially, 4,292 studies were retrieved from the search, of which 24 were excluded as duplicates. Titles and abstracts were screened for the remaining 4,268 studies, of which 4,239 were excluded due to the extraneous nature of the titles and/or abstracts. Subsequently, 29 full-text articles were assessed, and 19 were removed for lacking the outcome of interest and/or not satisfying the study’s inclusion criteria. Finally, 10 studies were included in the review, as shown in detail in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow-chart in Figure 1.
- Characteristics of selected studies
- The characteristics of the 10 included studies are described in Table 1. The plurality of the studies (4) were conducted in Australia [9-12], and one was conducted in each of the following countries: Sweden [13], India [14], Canada [15], Jordan [16], Germany [17], and Singapore [18]. Most of the studies utilized cross-sectional [13- 16] and retrospective study designs [9,11,12,18]. There was meaningful variation in the sample size across the included studies, ranging from 37 [17] to 1,720 [13]. In most of the studies, the mean age of the population was ≥ 65 years, except in 2 studies [14,16].
- Quality evaluation criteria
- The quality of the studies was assessed using the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields, which was developed by Kmet et al. [9]. The quality scores of most studies ranged from 80% to 100%, although 1 study [12] had the maximum score of 100% and 1 study [18] had a lower score (77%). Overall, the quality of the included studies was satisfactory. The quality scores of each study are presented in Table 2.
RESULTS
- HMR programs are emerging as one of the extended roles of community pharmacists in developed countries such as Australia, the USA, Canada, and various European countries [4,19,20]. Unfortunately, such programs have not been launched in most developing countries, such as India, for diverse reasons including the reluctance of general practitioners to follow recommendations made by pharmacists, a lack of awareness regarding HMR services among the public, patients’ conflicts of interest and privacy issues that affect their willingness to disclose their disease status and medication use, and linguistic and cultural diversity [5,6]. However, a few studies have investigated the influence of pharmacist-provided patient counseling services and found that such counseling services led to significant improvements in health outcomes in patients with chronic diseases [21-25]. The professional bodies in Australia have developed guidelines on HMR activities to assist community pharmacists in exercising professional judgment in individual health care circumstances and to promote the quality use of medicines to achieve better patient care. Diverse international studies of HMR services have reflected on optimizing medication use, minimizing DRPs, and improvising better health care outcomes in patients with chronic diseases and polypharmacy [26].
- In addition to improving health care outcomes by fostering an understanding of one’s medicines and the ability to manage those medicines appropriately, HMR services also provide recommendations for general practitioners on any potential DRPs that may affect patient safety [27]. A study conducted by Dhillon et al. [6] on general practitioners’ perceptions of HMR programs confirmed that HMR improved general practitioners’ knowledge of the medicines that their patients were taking. A study conducted by Turner et al. [26] in Australia assessed the benefits of HMR and stated that pharmacists identified expired and unwanted over-the-counter medications with the patients during the comprehensive medication review [26]. Another study conducted by Gilbert et al. [3] to assess the usefulness of an HMR collaborative service that included 1,000 patients with 129 general practitioners and 63 pharmacists identified that a significant number (2,900) of DRPs were identified, of which 17% were wrong medication selection and 20% were poor medication adherence due to an inadequate knowledge of the drug on the part of consumers; in that study, the collaborative efforts of general practitioners and pharmacists helped to resolve 85% of the DRPs [3].
- Besides identifying and resolving DRPs, HMR services provided by pharmacists could significantly decrease the rate of hospital readmission and its associated healthcare expenditures [18]. However, in a systematic review and meta-analysis conducted by Holland et al. [28], it was inferred that pharmacist-led medication review could reduce the number of drugs prescribed, and may improve patients’ drug-related knowledge and adherence behavior, but has no effect on mortality and morbidity. Furthermore, another study conducted by Pacini et al. [29] reported that HMR services provided by pharmacists did not reduce hospital admissions; instead, they observed only a minimal benefit in patients’ health-related quality of life that was not statistically significant.
- In a quantitative survey of the views of HMR recipients conducted by Carter et al. [30], respondents reported the highest level of agreement that HMR would be of help in understanding more about their medications and rated the interpersonal skills of the visiting pharmacist as extremely high. In another study that attempted to assess the willingness of caregivers to assist their carerecipients with HMR, it was concluded that building expectations of HMR as an information resource among informal caregivers would likely increase the overall consumer demand for this service, which may ease the stress and burden of caregiving [31]. An Australian survey of consumers’ perspectives on HMR reported that those with the greatest need of the services were the least likely to receive HMR, and that the service recipients were well-satisfied with the HMR and recognized the benefits of the process [27]. However, patient involvement and cooperation are essential for them to receive a benefit from HMR services. In this review, we have sought to summarize and encapsulate the diverse findings of studies addressing the role of pharmacists in offering HMR services in community home care settings. Nonetheless, this study has certain limitations, including the inability to evaluate the results through a meta-analysis due to the small number of studies and the diverse outcome measures assessed in those studies, as well as the exclusion of studies without full-text access [32-35]. Furthermore, not appraising the risk of publication bias is a drawback of this study.
DISCUSSION
- If utilized appropriately, HMR services provided by pharmacists could assist patients in minimizing and/or averting DRPs to a significant extent, especially among the elderly. To prevent medication accidents and to improve adherence among patients, it is necessary to implement HMR services, and necessary measures should be taken by health regulatory bodies to increase awareness of HMR and to make use of existing HMR tools among the public. However, further robust research should be conducted to evaluate the effects of HMR programs on reducing hospital admissions and emergency visits.
CONCLUSION
SUPPLEMENTARY MATERIALS
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTIONS
Conceptualization: SKG, KKT. Data curation: AK, MC, MR. Formal analysis: SKG, KKT, AK. Funding acquisition: None. Methodology: SKG, AK. Project administration: SKG, AK, KKT. Visualization: MC, MR. Writing – original draft: SKG, AK, KKT. Writing – review & editing: SKG.
NOTES
| Author, year, country, study design, sample size, and mean age | Aim of the study | Intervention(s) | Outcome(s) | Results and key findings | Summary |
|---|---|---|---|---|---|
| Basheti et al. [16], 2011, Jordan, cross-sectional study, 167 patients, 58.9 yr | To assess the prevalence of TRPs and their types among chronic disease patients | HMR by pharmacists. | Prevalence and nature of TRPs | The mean number of disease conditions and number of medications per patient were found to be 4.1 ± 1.7 and 8.1 ± 2.7, respectively; The mean number of TRPs identified per patient through the HMR was 7.4 ± 2.8; Among the TRPs identified, 125 (74.9%) were incomplete drug therapy problems, 114 (68.3%) were untreated conditions, 101 (60.5%) were non-adherence to non-pharmacological therapy, 84 (50.3%) were inappropriate dosage regimens, 40 (23.9%) were adverse drug effects, and the fewest were potential drug interactions (n=17; 10.2%) | The study results demonstrated the integral role of pharmacists in identifying TRPs in Jordanian outpatients with chronic diseases visiting community pharmacies; Furthermore, patients were satisfied and accepted the HMR services offered by their community pharmacists, including the home visit aspect |
| Castelino et al. [9], 2009, Australia, retrospective cohort study, 224 patients, 74.65 yr | To assess the nature and extent of DRPs and the actions recommended by the pharmacists to resolve DRPs | HMR by pharmacists. | DRPs | Patients who were receiving HMR services were prescribed a mean (SD) number of 10.7 (3.8) medications; Pharmacists identified at least 1 DRP in 98% of the patients reviewed; Overall, the pharmacists identified a total of 1,110 DRPs, the most common (16%) being the need for an additional medicine; On average (SD), 4.9 (2.9) problems were identified per patient; Thirty-four percent of all the problems were related to the selection of a specific medicine, 24% to the medication dosing regimen and management issues, and 19% to patients’ knowledge and medication management skills | The study infers that a well-trained pharmacist with full access to the patients and their medical records and supporting resources could potentially enhance the quality use of medicines among the elderly population; It also suggests that most of the actions recommended by the pharmacists during the HMR process were consistent with the current literature |
| Chandrasekar et al. [14], 2017, India, cross-sectional study, 85 patients, 40-59 yr | To identify, prevent, and resolve potential MROs, optimize pharmacotherapy, and assist in achieving better health outcomes for patients at home | HMR by pharmacists | MRPs | Drug interactions were the main problem found in the majority of the prescriptions; Around 32% of the population experienced ADRs upon taking medications, and 64% of them did not use any over-the-counter drugs; In terms of knowledge gaps, multiple drug storage was the most critical error, while 34% of the patients were not aware of the name of a drug, 27% did not know the reason for taking a drug, and 27% were not aware of individual instructions given during pregnancy | This study suggested that qualified pharmacists can play a major role in improving the appropriateness of prescribing and preventing medication-related adverse events; Additionally, pharmacists in collaboration with general practitioners can optimize patients’ medications |
| Cheen et al. [18], 2016, Singapore, retrospective cohort study, 499 patients, >70 yr | To determine the impact of a pharmacist-provided HBMR program on readmissions in the elderly population | HBMR by a pharmacist | DRPs, readmission rate, ED visits, outpatient visits, and mortality | A total of 464 DRPs, corresponding to an average of about 5 DRPs per patient, were identified; Pharmacist-provided HBMR reduced readmissions by 26%, reduced ED visits by 20%, and increased outpatient visits by 16%; The most commonly identified DRPs were non-adherence (38.6%), untreated indication (22.4%), and overdosage (9.9%), and the pharmacists had resolved 36.4% of DRPs within 1 month of the home visit | This study suggested that pharmacist-led HBMR services led to significantly decreased readmissions and emergency visits among the elderly population; However, the mortality benefit was unclear, although there was a trend towards lower mortality among those who received HBMR |
| Elliott et al. [10], 2012, Australia, prospective randomized comparative study, 80 patients, 84 yr | To compare 3 different methods for promoting a pharmacist-led medication review for patients referred to an ACAT and to compare MRPs identified via ACAT usual care with those identified via pharmacist-led medication reviews | Comprehensive medication review by pharmacists | MRPs | Overall, 21 MRPs were identified via ACAT usual care: 5 (23.8%) were classified as high-risk, 10 (47.6%) as moderate-risk, 5 (23.8%) as low-risk, and 1 (4.8%) as insignificant; Pharmacists’ review of the ACAT files (without a pharmacist home visit) identified a further 164 potential MRPs; however, in the 40 patients who received an APHMR, 35 of 82 potential MRPs (42.7%) turned out not to be actual problems once further information was obtained from the patient; The APHMR identified 79 additional MRPs that were not identified from a review of the ACAT files; In total, 122 pharmacist-identified MRPs were included in APHMR reports to patients’ GPs; 94 of these were assessed as being associated with moderate, high, or extreme risk of an adverse event if not addressed | The study revealed that adding a pharmacist to the usual care assessment teams could significantly help in identifying and resolving MRPs; In addition, it was also inferred that home visits by a pharmacist can serve as a more efficient way for identifying MRPs than a routine medication review of the collected data; Furthermore, adding pharmacists to ACATs may provide a reliable and cost-effective method for delivering medication reviews, which reduce the risk of adverse events |
| Fiss et al. [17], 2010, Germany, prospective cohort study, 37 patients, 75.5 yr | To establish an interdisciplinary health professional network to systematically identify and evaluate DRPs in the patients’ homes, and to provide recommendations | Community-based HMR | DDIs | During a GP–supporting, community-based, e-health assisted, systemic intervention, 56 potential DDIs were identified, and 37 of the 112 drugs which caused potential interactions were attributed to OTC medication and food components; The mean number of drugs recorded per patient was 14.2; The evaluations of clinically relevant potential DDIs yielded relevant DDIs in 44.6% of the patients (n=25) | The study results suggested that a notable prevalence of DRPs was identified by a comprehensive HMR conducted by GP–supporting, community-based, e-health assisted, systemic intervention practice assistants in cooperation with local pharmacists |
| Gheewala et al. [12], 2014, Australia, retrospective cohort study, 847 patients, 84.9 yr | To investigate the number and nature of DRPs and recommendations made by pharmacists among residents of aged care facilities | Collaborative RMMR service by pharmacists | DRPs | Of the 847 included patients, the mean (SD) number of medications prescribed per resident was 11.2 (4.8); The pharmacists identified a total of 2,712 DRPs in 98% of the residents; The mean (SD) number of DRPs identified per resident was 3.2 (1.7); Of 3,054 recommendations made, 2,560 (83.8%) were accepted by the GP; The mean (SD) number of recommendations made per resident by the pharmacist was 3.6 (1.9) and mean (SD) number of recommendations accepted by the GP per resident was 3.0 (1.9) | The study suggested that the collaborative RMMR service with the help of an accredited pharmacist could significantly reduce DRPs among the residents of aged care facilities |
| Lenander et al. [13], 2018, Sweden, cross-sectional study, 1,720 patients, 87.5 yr | To evaluate the effect of medication reviews on total medication use and potentially inappropriate drug use among elderly patients, and to describe the occurrence and types of DRPs | Medication review by clinical pharmacists | DRPs | Of the 1,720 patients, 61% of them were on 10 or more drugs (range, 1-35); DRPs were identified in 84% of the patients, and a total of 3,868 DRPs were identified, giving a mean of 2.2 DRPs per patient; The most frequent types of DRPs (n = 3,868) identified were unnecessary drug therapy (39%), the wrong drug (20%), and an excessively high dose of medications (21%); Drug withdrawal was identified as the most common result | This study inferred that medication reviews performed in daily care by clinical pharmacists are one way to identify DRPs and to improve drug use among elderly patients; It also concluded that drug use is voluminous among elderly patients in home care and nursing home residents, and that additional drug therapy is a common problem |
| Nishtala et al. [11], 2009, Australia, retrospective cohort study, 500 patients, 84 yr | To investigate the number and nature of DRPs identified by accredited clinical pharmacists | Medication review by accredited clinical pharmacists. | DRPs | In a 500 randomly selected, de-identified medication reviews performed by 10 accredited clinical pharmacists over 6 months across 62 aged care homes, a total of 1,433 MRPs were identified in 480 residents; Potential DRPs were classified as a need for additional monitoring, risk of ADRs, and inappropriate choice of a drug; Among identified DRPs, alimentary, cardiovascular, central nervous system and respiratory drugs were most frequently implicated, accounting for more than 75% of the DRPs | The study concluded that clinical pharmacists have a potential role in identifying DRPs among older people living in aged care homes; Moreover, the recommendations made by pharmacists to minimize the risk of ADRs and to optimize drug choices were accepted and implemented by GPs |
| Papastergiou et al. [15], 2013, Canada, cross-sectional study, 43 patients, 77.4 yr | To identify and resolve the drug therapy problems of homebound patients | Pharmacist-directed HMR | Drug-therapy problems | The patients were taking a mean of 11.7 (range, 3-23) medications; Pharmacists identified a total of 62 drug therapy problems; The top 3 types of problems identified were non-compliance (40.3%), ADRs (20.9%) and additional therapy required (19.4%); Of the seniors, 44% were found to be using at least 1 medication on the Beers criteria list, whereas 7% were using 3 or more; Medications were removed from the homes of 58% of the patients, most commonly due to expiry of medication | The study concluded that pharmacists are among the most accessible front-line primary care practitioners and can provide care to home-bound patients; Pharmacist-directed HMRs offer an effective mechanism to address pharmacotherapy issues and could serve to minimize the inappropriate use of medication and health care costs |
TRPs, treatment-related problems; HMR, home medications review; DRPs, drug-related problems; SD, standard deviation; ADRs, adverse drug reactions; HBMR, home-based medication review; ED, emergency department; ACAT, aged care assessment team; MRPs, medication-related problems; APHMR, ACAT-initiated pharmacist home medicines review; DDIs, drug-drug interactions; OTC, over-the-counter; GP, general practitioner; RMMR, residential medication management review.
| Criteria |
Study |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| [9] | [10] | [17] | [18] | [11] | [13] | [12] | [14] | [15] | [16] | |
| Question/objective sufficiently described? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Study design evident and appropriate? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Method of subject/comparison group selection or source of information/input variables described and appropriate? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 |
| Subject (and comparison group, if applicable) characteristics sufficiently described? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 |
| If interventional and random allocation was possible, was it described? | N/A | 2 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| If interventional and blinding of investigators was possible, was it reported? | N/A | 0 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| If interventional and blinding of subjects was possible, was it reported? | N/A | 2 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Outcome and (if applicable) exposure measure(s) well defined and robust to measurement / misclassification bias? Means of assessment reported? | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Sample size appropriate? | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 1 | 2 |
| Analytic methods described/justified and appropriate? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 |
| Is some estimate of variance is reported for the main results? | 0 | 2 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| Controlled for confounding? | N/A | 0 | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Results reported in sufficient detail? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Conclusions supported by the results? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Maximum points | 20 | 28 | 22 | 22 | 20 | 20 | 20 | 20 | 20 | 20 |
| Total points | 18 | 24 | 17 | 21 | 20 | 18 | 18 | 16 | 16 | 18 |
| Summary score (%) | 90 | 86 | 77 | 95 | 100 | 90 | 90 | 80 | 80 | 90 |
- 1. Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother 2007;5:345-351.ArticlePubMed
- 2. Castelino RL, Bajorek BV, Chen TF. Retrospective evaluation of home medicines review by pharmacists in older Australian patients using the medication appropriateness index. Ann Pharmacother 2010;44:1922-1929.ArticlePubMed
- 3. Gilbert AL, Roughead EE, Beilby J, Mott K, Barratt JD. Collaborative medication management services: improving patient care. Med J Aust 2002;177:189-192.ArticlePubMed
- 4. Willis JS, Hoy RH, Jenkins WD. In-home medication reviews: a novel approach to improving patient care through coordination of care. J Community Health 2011;36:1027-1031.ArticlePubMedPDF
- 5. Ahn J, Park JE, Anthony C, Burke M. Understanding, benefits and difficulties of home medicines review-patients’ perspectives. Aust Fam Physician 2015;44:249-253.PubMed
- 6. Dhillon AK, Hattingh HL, Stafford A, Hoti K. General practitioners’ perceptions on home medicines reviews: a qualitative analysis. BMC Fam Pract 2015;16:16.ArticlePubMedPMCPDF
- 7. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016;5:210.ArticlePubMedPMC
- 8. Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton: Alberta Heritage Foundation for Medical Research; 2004. p 1-22.
- 9. Castelino RL, Bajorek BV, Chen TF. Are interventions recommended by pharmacists during home medicines review evidence‐based? J Eval Clin Pact 2011;17:104-110.Article
- 10. Elliott RA, Martinac G, Campbell S, Thorn J, Woodward MC. Pharmacist-led medication review to identify medication-related problems in older people referred to an Aged Care Assessment Team: a randomized comparative study. Drugs Aging 2012;29:593-605.ArticlePubMedPDF
- 11. Nishtala PS, McLachlan AJ, Bell JS, Chen TF. A retrospective study of drug‐related problems in Australian aged care homes: medication reviews involving pharmacists and general practitioners. J Eval Clin Pract 2011;17:97-103.ArticlePubMed
- 12. Gheewala PA, Peterson GM, Curtain CM, Nishtala PS, Hannan PJ, Castelino RL. Impact of the pharmacist medication review services on drug-related problems and potentially inappropriate prescribing of renally cleared medications in residents of aged care facilities. Drugs Aging 2014;31:825-835.ArticlePubMedPDF
- 13. Lenander C, Bondesson Å, Viberg N, Beckman A, Midlöv P. Effects of medication reviews on use of potentially inappropriate medications in elderly patients; a cross-sectional study in Swedish primary care. BMC Health Serv Res 2018;18:616.ArticlePubMedPMCPDF
- 14. Chandrasekhar D, Joseph E, Ghaffoor FA, Thomas HM. Role of pharmacist led home medication review in community setting and the preparation of medication list. Clin Epidemiol Glob Health 2019;7:66-70.Article
- 15. Papastergiou J, Zervas J, Li W, Rajan A. Home medication reviews by community pharmacists: reaching out to homebound patients. Can Pharm J 2013;146:139-142.Article
- 16. Basheti IA, Qunaibi EA, Bulatova NR, Samara S, AbuRuz S. Treatment related problems for outpatients with chronic diseases in Jordan: the value of home medication reviews. Int J Clin Pharm 2013;35:92-100.ArticlePubMedPDF
- 17. Fiss T, Ritter CA, Alte D, van den Berg N, Hoffmann W. Detection of drug related problems in an interdisciplinary health care model for rural areas in Germany. Pharm World Sci 2010;32:566-574.ArticlePubMedPDF
- 18. Cheen MH, Goon CP, Ong WC, Lim PS, Wan CN, Leong MY, et al. Evaluation of a care transition program with pharmacist-provided home-based medication review for elderly Singaporeans at high risk of readmissions. Int J Qual Health Care 2017;29:200-205.ArticlePubMed
- 19. Quirke J, Wheatland B, Gilles M, Howden A, Larson A. Home medicines reviews - do they change prescribing and patient/pharmacist acceptance? Aust Fam Physician 2006;35:266-267.PubMed
- 20. Elina AN, Suraya MC, Ball PA. The impact of home medication review in patients with type 2 diabetes mellitus living in rural areas of Kuantan, Malaysia. Value Health 2014;17:A127.Article
- 21. Srinivas B, Shivram G, Swapnali M, Pratibha C, Sagar B, Kailash V. Betterment of patient to get optimal health outcomes through home medicines review (HMR). Int J Pharm Res Allied Sci 2014;3:10-16.
- 22. Mishra A, Krishna GS, Alla S, Kurian TD, Kurian J, Ramesh M, et al. Impact of pharmacist–psychiatrist collaborative patient education on medication adherence and quality of life (QOL) of Bipolar Affective Disorder (BPAD) patients. Front Pharmacol 2017;8:722.ArticlePubMedPMC
- 23. Mishra A, Krishna GS, Sravani A, Kurian TD, Kurian J, Ramesh M, et al. Impact of pharmacist-led collaborative patient education on medication adherence and quality of life of schizophrenia patients in a tertiary care setting. Bull Fac Pharm Cairo Univ 2017;55:345-349.Article
- 24. Gudi SK. Assessment of knowledge, attitude and perceptions of HIV/AIDS among secondary school students in Guntur district of south India: a cross-sectional survey. Int J Sci Rep 2018;4:87-92.Article
- 25. Gudi SK, Chhabra M, Rashid M. Assessment of the impact of pharmacist-led face-to-face counselling on HIV/AIDS among school & college going students, and infected patients in south India. Clin Epidemiol Glob Health 2019;doi: https://doi.org/10.1016/j.cegh.2019.01.006.ArticlePubMedPMC
- 26. Turner JP, Bell JS. Implementation of pharmacist-led medication reviews in general practice. Int J Clin Pharm 2013;35:3-4.ArticlePubMedPDF
- 27. White L, Klinner C, Carter S. Consumer perspectives of the Australian Home Medicines Review Program: benefits and barriers. Res Social Adm Pharm 2012;8:4-16.ArticlePubMed
- 28. Holland R, Desborough J, Goodyer L, Hall S, Wright D, Loke YK. Does pharmacist‐led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta‐analysis. Br J Clin Pharmacol 2008;65:303-316.ArticlePubMed
- 29. Pacini M, Smith RD, Wilson EC, Holland R. Home-based medication review in older people: is it cost effective? Pharmacoeconomics 2007;25:171-180.ArticlePubMed
- 30. Carter SR, Chen TF, White L. Home medicines reviews: a quantitative study of the views of recipients and eligible non-recipients. Int J Pharm Pract 2012;20:209-217.ArticlePubMed
- 31. Carter SR, Moles R, White L, Chen TF. The willingness of informal caregivers to assist their care-recipient to use home medicines review. Health Expect 2016;19:527-542.ArticlePubMed
- 32. Steele KM, Ruisinger JF, Bates J, Prohaska ES, Melton BL, Hipp S. Home-based comprehensive medication reviews: pharmacist’s impact on drug therapy problems in geriatric patients. Consult Pharm 2016;31:598-605.ArticlePubMed
- 33. Alderman CP, Kong L, Kildea L. Medication-related problems identified in home medicines reviews conducted in an Australian rural setting. Consult Pharm 2013;28:432-442.ArticlePubMed
- 34. Vink J, Morton D, Ferreri S. Pharmacist identification of medication-related problems in the home care setting. Consult Pharm 2011;26:477-484.ArticlePubMed
- 35. Stuijt CC, Franssen EJ, Egberts AC, Hudson SA. Appropriateness of prescribing among elderly patients in a Dutch residential home: observational study of outcomes after a pharmacist-led medication review. Drugs Aging 2008;25:947-954.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Drug-Related Problems and Sick Day Management Considerations for Medications that Contribute to the Risk of Acute Kidney Injury
Mimi Truong, Wubshet Tesfaye, Kamal Sud, Connie Van, Shrey Seth, Nerida Croker, Ronald Lynel Castelino
Journal of Clinical Medicine.2024; 13(2): 343. CrossRef - Informing policy makers in developing countries: Practices and limitations of geriatric home medication review in Malaysia-A qualitative inquiry
Ahlam Sundus, Renukha Sellappans, Tan Maw Pin
Asian Pacific Journal of Tropical Medicine.2024; 17(1): 21. CrossRef - Evaluation of a pharmacist-led intervention to reduce drug-related problems in patients included in a home healthcare program: study protocol for a pragmatic randomized clinical trial
Clara Salom-Garrigues, Enric Aragonès, Montse Giralt, Cecília Campabadal Prats, Ferran Bejarano-Romero, Laura Canadell
BMC Geriatrics.2024;[Epub] CrossRef - Medication Review: What’s in a Name and What Is It about?
Anneleen Robberechts, Maja Brumer, Victoria Garcia-Cardenas, Niurka M. Dupotey, Stephane Steurbaut, Guido R. Y. De Meyer, Hans De Loof
Pharmacy.2024; 12(1): 39. CrossRef - Drug-Related Problems and Recommendations Made during Home Medicines Reviews for Sick Day Medication Management in Australia
Mimi Truong, Connie Van, Kamal Sud, Wubshet Tesfaye, Nerida Croker, Shrey Seth, Ronald Lynel Castelino
Medicina.2024; 60(5): 798. CrossRef - Assessment of a Geriatric Evaluation and Management in the Home (GEMITH) Service at a Quaternary Hospital: A Retrospective Observational Study
Keshia R. De Guzman, Duncan Long, Alexander Theodos, Alexandra Karlovic, Nazanin Falconer
Journal of Pharmacy Practice.2024;[Epub] CrossRef - Investigating the value of medication management review for asthma patients: A randomized controlled study
Tahani Tawfiq Al-Bahnasi, Iman Basheti
Electronic Journal of General Medicine.2024; 21(3): em594. CrossRef - Development and trial of an instrument to evaluate accredited pharmacists' clinical home medicines review reports in Australia
Marea Patounas, Esther T. L. Lau, Deborah Rigby, Vincent Chan, Lisa M. Nissen
Journal of Pharmacy Practice and Research.2023; 53(1): 32. CrossRef - Clinical impact of medication reviews for community-dwelling patients in primary healthcare
Annika Dobszai, Cecilia Lenander, Beata Borgström Bolmsjö, Katarina Wickman, Sara Modig
BMC Primary Care.2023;[Epub] CrossRef - The effect of home medication review in community-dwelling older adults: a systematic review
Sarah M. Abu Fadaleh, Theresa L. Charrois, Tatiana Makhinova, Dean T. Eurich, Sholeh Rahman, Cheryl A. Sadowski
Journal of Public Health.2022; 30(8): 1857. CrossRef - Impact of pharmacist-led shared medication reviews on adherence among polymedicated older patients: an observational retrospective French study
Gersende Faton, Pierre-Antoine Drubay, Geoffroy Vergez, Sébastien Faure
Journal of the American Pharmacists Association.2022; 62(1): 150. CrossRef - Effects of home medication review on drug-related problems and health-related quality of life among community-dwelling older adults in China
Sha Zhang, Deqiu Zhu, Zhan Qi, Lulu Tian, Shijing Qian, Danfei Song, Beilei Chen, Shanshan Tong, Jing Wang, Juan Wu
Journal of the American Pharmacists Association.2022; 62(2): 481. CrossRef - Drug therapy-related problem management in Nigeria community pharmacy – process evaluation with simulated patient
Showande Johnson Segun, Lawal Sodiq Damilola
BMC Health Services Research.2022;[Epub] CrossRef - Identifying Potential Drug-Related Problems Among Geriatric Patients With Use of an Integrated Clinical Decision Support Tool
Veera Bobrova, Daniela Fialová, Shane Desselle, Jyrki Heinämäki, Daisy Volmer
Frontiers in Pharmacology.2022;[Epub] CrossRef - What Is the Medication Iatrogenic Risk in Elderly Outpatients for Chronic Pain?
Julie Jambon, Chloé Choukroun, Clarisse Roux-Marson, Éric Viel, Géraldine Leguelinel-Blache
Clinical Neuropharmacology.2022; 45(3): 65. CrossRef - Home medication management problems and associated factors among psychiatric patients using home care pharmacy services at government hospitals in western Malaysia
Christine Li Ling Lau, Cheah Yen Hor, Siew Ting Ong, Muhammad Fadhlullah Roslan, Xin Yi Beh, Dashnilatha Permal, Shamini Rama
BMC Health Services Research.2022;[Epub] CrossRef - The value of domiciliary medication reviews – a thematic analysis of pharmacist’s views
Patricia McCormick, Bridget Coleman, Ian Bates
International Journal of Clinical Pharmacy.2022; 44(4): 1004. CrossRef - Polypharmacy in the Homebound Population
Erin Atkinson Cook, Maria Duenas, Patricia Harris
Clinics in Geriatric Medicine.2022; 38(4): 685. CrossRef - Applicability of tools to identify potentially inappropriate prescribing in elderly during medication review: Comparison of STOPP/START version 2, Beers 2019, EU(7)-PIM list, PRISCUS list, and Amsterdam tool—A pilot study
Agnieszka Lisowska, Edyta Czepielewska, Martyna Rydz, Anna Dworakowska, Magdalena Makarewicz-Wujec, Małgorzata Kozłowska-Wojciechowska, Antonio De Vincentis
PLOS ONE.2022; 17(9): e0275456. CrossRef - Impact of pharmacist care in the management of autoimmune disorders: A systematic review of randomized control trials and non-randomized studies
Sujit Kumar Sah, Subramanian R, Madhan Ramesh, Sharad Chand
Research in Social and Administrative Pharmacy.2021; 17(9): 1532. CrossRef - A systematic review of general practice-based pharmacists’ services to optimize medicines management in older people with multimorbidity and polypharmacy
Ameerah S Hasan Ibrahim, Heather E Barry, Carmel M Hughes
Family Practice.2021; 38(4): 509. CrossRef - Economic evaluation of home medication review by community pharmacists (HMR-CP) for patients with type 2 diabetes mellitus (T2DM)
Mohd Rozaini Rosli, David Bin-Chia Wu, Chin Fen Neoh, Mahmathi Karuppannan
Journal of Medical Economics.2021; 24(1): 730. CrossRef - The value of domiciliary medication reviews: a thematic analysis of patient views
Patricia McCormick, Bridget Coleman, Ian Bates
International Journal of Clinical Pharmacy.2021; 43(6): 1594. CrossRef - Impact Analysis of a Pharmacist-Led Home-Medication Review Service Within an Interprofessional Outreach Team
Wuqi Lin, Sabrina Haq, Samir Sinha, Chris Fan-Lun
The Senior Care Pharmacist.2021; 36(3): 159. CrossRef - Clinical and Humanistic Outcomes of Community Pharmacy-Based Healthcare Interventions Regarding Medication Use in Older Adults: A Systematic Review and Meta-Analysis
Christina Malini Christopher, Bhuvan KC, Ali Blebil, Deepa Alex, Mohamed Izham Mohamed Ibrahim, Norhasimah Ismail, Alian A. Alrasheedy
Healthcare.2021; 9(11): 1577. CrossRef - How Do Pharmacists Practice in Aged Care? A Narrative Review of Models from Australia, England, and the United States of America
Ibrahim Haider, Mark Naunton, Rachel Davey, Gregory M. Peterson, Wasim Baqir, Sam Kosari
International Journal of Environmental Research and Public Health.2021; 18(23): 12773. CrossRef - Opportunities for changes in the drug product design to enhance medication safety in older people: Evaluation of a national public portal for medication incidents
Fatma Karapinar‐Çarkit, Patricia M.L.A. van den Bemt, Mariam Sadik, Brigit van Soest, Wilma Knol, Florence van Hunsel, Diana A. van Riet‐Nales
British Journal of Clinical Pharmacology.2020; 86(10): 1946. CrossRef - Clinic- and Hospital-Based Home Care, Outpatient Parenteral Antimicrobial Therapy (OPAT) and the Evolving Clinical Responsibilities of the Pharmacist
Toni Docherty, Jennifer J. Schneider, Joyce Cooper
Pharmacy.2020; 8(4): 233. CrossRef

 KSE
KSE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite


