Impact of pharmacist-led home medicines review services on drug-related problems among the elderly population: a systematic review
Article information
Abstract
OBJECTIVES
To address and elucidate the impact of pharmacist-led home medicines review (HMR) services on identifying drug-related problems (DRPs) among the elderly population in home care settings.
METHODS
A comprehensive systematic search was performed using electronic scientific databases such as PubMed, Scopus, Embase, and Web of Science for studies published between January 1, 2008 and December 31, 2018, pertaining to HMR services by pharmacists for identifying DRPs.
RESULTS
In total, 4,292 studies were retrieved from the searches, of which 24 were excluded as duplicates. Titles and abstracts were screened for the remaining 4,268 studies, of which 4,239 were excluded due to the extraneous nature of the titles and/or abstracts. Subsequently, 29 full-text articles were assessed, and 19 were removed for lacking the outcome of interest and/or not satisfying the study’s inclusion criteria. Finally, 10 studies were included in the review; however, publication bias was not assessed, which is a limitation of this study. In all studies, pharmacists identified a highly significant amount of DRPs through HMR services. The most common types of DRPs were potential drug-drug interactions, serious adverse drug reactions, need for an additional drug, inappropriate medication use, non-adherence, untreated indications, excessive doses, and usage of expired medications.
CONCLUSIONS
HMR is a novel extended role played by pharmacists. The efficiency of such programs in identifying and resolving DRPs could minimize patients’ health-related costs and burden, thereby enhancing the quality of life and well-being among the elderly.
INTRODUCTION
In countries with numerous and diverse populations, chronic diseases such as hypertension, diabetes, arthritis, and heart disease are common, especially among geriatric individuals; as a result, polypharmacy is a frequently occurring phenomenon in the elderly. Polypharmacy may give rise to various drug-related problems (DRPs), such as drug-drug interactions, adverse drug reactions (ADRs), medication errors, and drug-food interactions, which could eventually reduce levels of medication adherence [1]. At times, elderly patients might not take their medications as prescribed, which could evolve into altering the dose, frequency, or terminating the medication itself. The reasons for this may vary from simple logistical misunderstandings of factors such as the appropriate timing and dosage to a deeper misunderstanding of the purpose of a medication. Thus, inappropriate medication use among this vulnerable population is a major health concern [2]. ADRs are a major burden to patients, as shown by the fact that they are considered the fifth most common cause of death amongst hospitalized patients, with a notable morbidity rate of 5.6% in India. Therefore, several studies have been conducted to develop strategies for minimizing and preventing DRPs, including home medicines review (HMR) programs [3,4].
In 2001, the Australian government initiated the first HMR program, defined as a consumer-focused, structured, and collaborative health care service in the community setting to promote better medication adherence [5]. It is a team-based approach that involves a clinician, pharmacist, and consumer to optimize the quality use of medicines and to improve consumers’ understanding of their medications. HMR starts with a referral by a clinician, which enables the pharmacist to visit the patient’s home in order to review the current medication therapy of that particular patient, to check for potential DRPs, and to resolve them in consultation with the responsible clinician [1,2]. The essential goal of the HMR program is to reduce the DRPs that are derived from inappropriate use of medicines, as doing so could enhance patients’ medication adherence [6]. In this review, we sought to critically inspect studies of the effects of pharmacist-initiated HMR programs on identifying and mitigating DRPs.
MATERIALS AND METHODS
Data sources and search strategy
A comprehensive search was performed of PubMed, Scopus, Embase, and Web of Science for peer-reviewed, full-text articles published in the English language between January 1, 2008 and December 31, 2018. Relevant keywords such as “HMR,” “home medicines review,” “drug related problems,” “pharmacist,” and “elderly” were searched in diverse combinations with Medical Subject Headings (MeSH) terms by using Boolean operators to identify all relevant studies. The detailed search strategy interpretation using PubMed was as follows: (“HMR” [All Fields] OR “home medicines review” [All Fields]) AND “drug-related problems” [All Fields] AND “pharmacists” [MeSH Terms] OR “pharmacists” [All Fields] AND (“aged” [MeSH Terms] OR “aged” [All Fields] OR “elderly” [All Fields]) AND (“2008/01/01” [PDAT]: “2018/12/31” [PDAT]). Any further missing publications were searched by checking the references of the included studies. ProQuest, Google Scholar, and Open Grey were searched for the grey literature.
Study selection and data extraction
Three reviewers (SKG, AK, and MC) independently screened the title and abstract of each article, and the potentially eligible full-texts of relevant abstracts were obtained and screened to identify articles of interest based on the study’s inclusion criteria, which were studies (prospective, retrospective, cross-sectional, or randomized) evaluating the impact of pharmacist-led HMR services on identifying DRPs among the elderly population. Articles were excluded if the outcome data were not reported in enough detail, the participants were not elderly, and the studies were conducted elsewhere from home or home care facilities; additionally, duplicate publications, literature reviews, conference abstracts, studies with no pharmacist involvement, and editorials/letters to the editor were excluded. The retrieved studies were imported into the Rayyan software [7] to remove duplicates and to review studies based on the inclusion and exclusion criteria. From each included study, the following data were extracted: author name(s), publication year, country, study design, sample size, mean age of the participants, key findings, and the summary. Any disagreements amongst the researchers regarding the inclusion of the studies were resolved through consensus, and a priori protocol was developed, and can be found in the Supplementary Material 1.
Risk of bias and quality assessment
The risk of bias and methodological quality of each included study were assessed by 2 independent reviewers (AK and SKG) using the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields [8], a 14-item measurement tool used to assess the methodological quality of the studies in a systematic review. Each item/question was scored as 2 (if the response was ‘yes’), 1 (if the response was ‘partial’), or 0 (if the response was ‘no’). Questions that were not applicable to a particular study were marked as ‘n/a’ and were excluded from the calculation of the summary score, which was calculated for each paper by summing the total score obtained for all items and dividing it by the total possible score. A higher summary score indicated a lower risk of bias and better study quality. Disagreements were resolved by discussions or by a third reviewer.
Outcome assessment
The outcome of interest of this review was DRPs, which were assessed in terms of their frequency, type, and nature as described in each included study. DRPs were defined as an event or circumstance involving drug therapy that potentially interfered with desired health outcomes.
RESULTS
Initially, 4,292 studies were retrieved from the search, of which 24 were excluded as duplicates. Titles and abstracts were screened for the remaining 4,268 studies, of which 4,239 were excluded due to the extraneous nature of the titles and/or abstracts. Subsequently, 29 full-text articles were assessed, and 19 were removed for lacking the outcome of interest and/or not satisfying the study’s inclusion criteria. Finally, 10 studies were included in the review, as shown in detail in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow-chart in Figure 1.
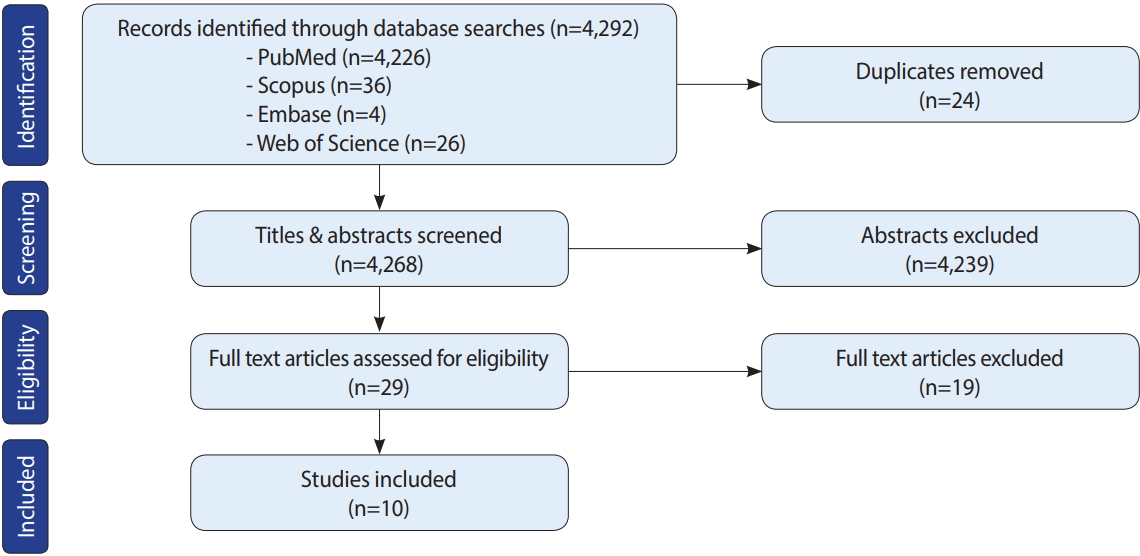
Preferred Reporting Items for System reviews and Meta-Analyses (PRISMA) flow-chart depicting the study selection process.
Characteristics of selected studies
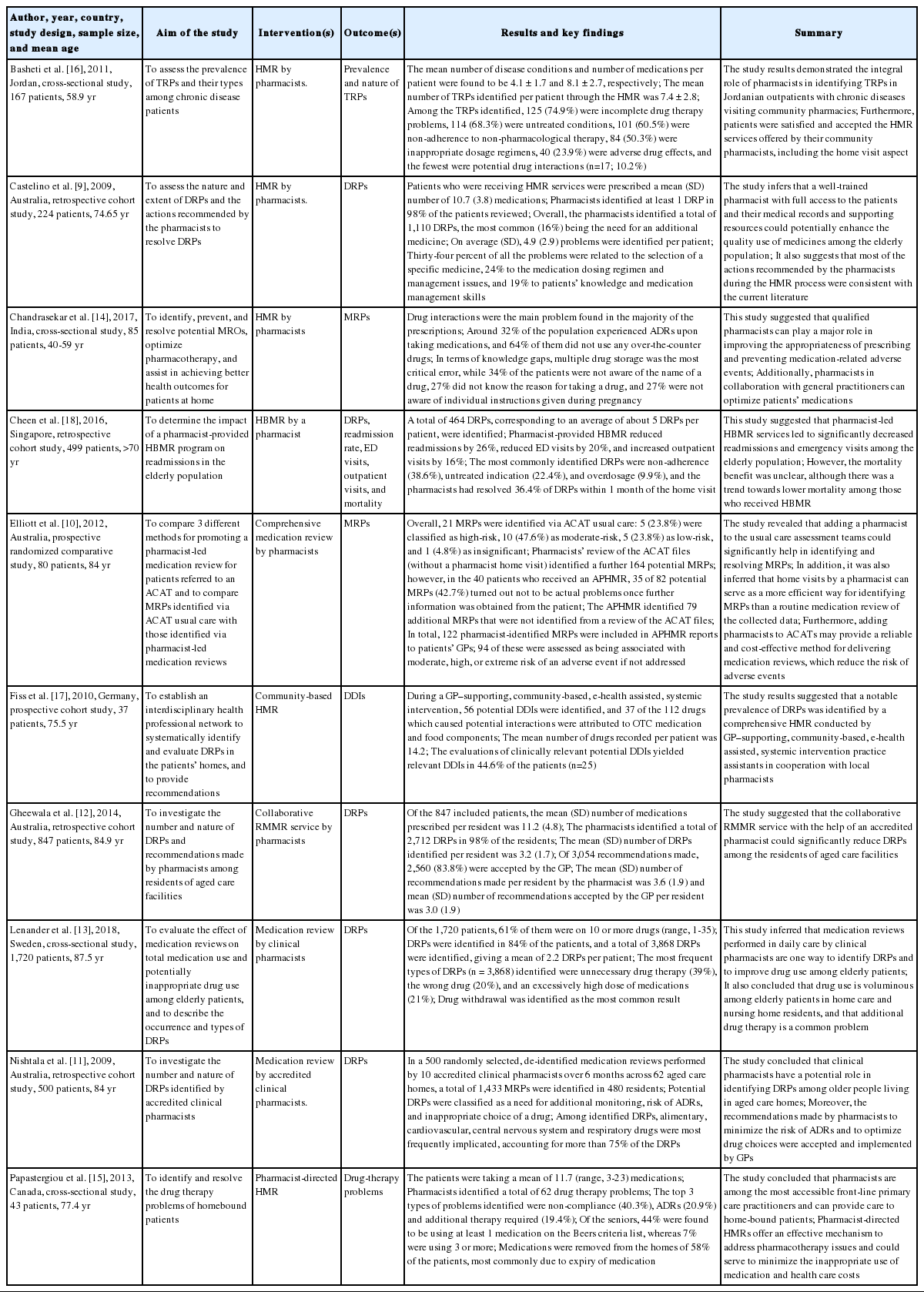
The characteristics of the 10 included studies are described in Table 1. The plurality of the studies (4) were conducted in Australia [9-12], and one was conducted in each of the following countries: Sweden [13], India [14], Canada [15], Jordan [16], Germany [17], and Singapore [18]. Most of the studies utilized cross-sectional [13- 16] and retrospective study designs [9,11,12,18]. There was meaningful variation in the sample size across the included studies, ranging from 37 [17] to 1,720 [13]. In most of the studies, the mean age of the population was ≥ 65 years, except in 2 studies [14,16].
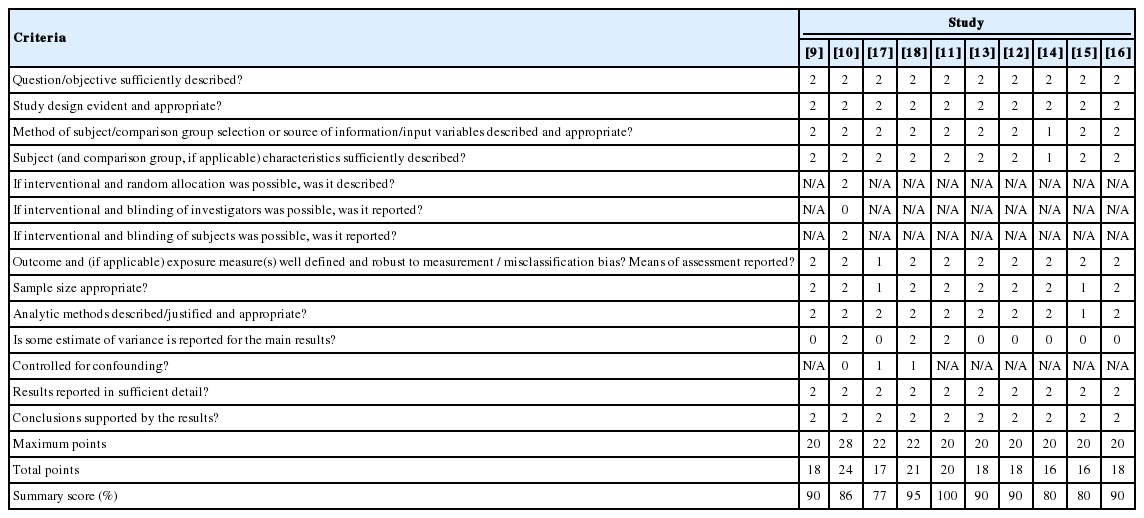
Quality evaluation criteria
The quality of the studies was assessed using the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields, which was developed by Kmet et al. [9]. The quality scores of most studies ranged from 80% to 100%, although 1 study [12] had the maximum score of 100% and 1 study [18] had a lower score (77%). Overall, the quality of the included studies was satisfactory. The quality scores of each study are presented in Table 2.
DISCUSSION
HMR programs are emerging as one of the extended roles of community pharmacists in developed countries such as Australia, the USA, Canada, and various European countries [4,19,20]. Unfortunately, such programs have not been launched in most developing countries, such as India, for diverse reasons including the reluctance of general practitioners to follow recommendations made by pharmacists, a lack of awareness regarding HMR services among the public, patients’ conflicts of interest and privacy issues that affect their willingness to disclose their disease status and medication use, and linguistic and cultural diversity [5,6]. However, a few studies have investigated the influence of pharmacist-provided patient counseling services and found that such counseling services led to significant improvements in health outcomes in patients with chronic diseases [21-25]. The professional bodies in Australia have developed guidelines on HMR activities to assist community pharmacists in exercising professional judgment in individual health care circumstances and to promote the quality use of medicines to achieve better patient care. Diverse international studies of HMR services have reflected on optimizing medication use, minimizing DRPs, and improvising better health care outcomes in patients with chronic diseases and polypharmacy [26].
In addition to improving health care outcomes by fostering an understanding of one’s medicines and the ability to manage those medicines appropriately, HMR services also provide recommendations for general practitioners on any potential DRPs that may affect patient safety [27]. A study conducted by Dhillon et al. [6] on general practitioners’ perceptions of HMR programs confirmed that HMR improved general practitioners’ knowledge of the medicines that their patients were taking. A study conducted by Turner et al. [26] in Australia assessed the benefits of HMR and stated that pharmacists identified expired and unwanted over-the-counter medications with the patients during the comprehensive medication review [26]. Another study conducted by Gilbert et al. [3] to assess the usefulness of an HMR collaborative service that included 1,000 patients with 129 general practitioners and 63 pharmacists identified that a significant number (2,900) of DRPs were identified, of which 17% were wrong medication selection and 20% were poor medication adherence due to an inadequate knowledge of the drug on the part of consumers; in that study, the collaborative efforts of general practitioners and pharmacists helped to resolve 85% of the DRPs [3].
Besides identifying and resolving DRPs, HMR services provided by pharmacists could significantly decrease the rate of hospital readmission and its associated healthcare expenditures [18]. However, in a systematic review and meta-analysis conducted by Holland et al. [28], it was inferred that pharmacist-led medication review could reduce the number of drugs prescribed, and may improve patients’ drug-related knowledge and adherence behavior, but has no effect on mortality and morbidity. Furthermore, another study conducted by Pacini et al. [29] reported that HMR services provided by pharmacists did not reduce hospital admissions; instead, they observed only a minimal benefit in patients’ health-related quality of life that was not statistically significant.
In a quantitative survey of the views of HMR recipients conducted by Carter et al. [30], respondents reported the highest level of agreement that HMR would be of help in understanding more about their medications and rated the interpersonal skills of the visiting pharmacist as extremely high. In another study that attempted to assess the willingness of caregivers to assist their carerecipients with HMR, it was concluded that building expectations of HMR as an information resource among informal caregivers would likely increase the overall consumer demand for this service, which may ease the stress and burden of caregiving [31]. An Australian survey of consumers’ perspectives on HMR reported that those with the greatest need of the services were the least likely to receive HMR, and that the service recipients were well-satisfied with the HMR and recognized the benefits of the process [27]. However, patient involvement and cooperation are essential for them to receive a benefit from HMR services. In this review, we have sought to summarize and encapsulate the diverse findings of studies addressing the role of pharmacists in offering HMR services in community home care settings. Nonetheless, this study has certain limitations, including the inability to evaluate the results through a meta-analysis due to the small number of studies and the diverse outcome measures assessed in those studies, as well as the exclusion of studies without full-text access [32-35]. Furthermore, not appraising the risk of publication bias is a drawback of this study.
CONCLUSION
If utilized appropriately, HMR services provided by pharmacists could assist patients in minimizing and/or averting DRPs to a significant extent, especially among the elderly. To prevent medication accidents and to improve adherence among patients, it is necessary to implement HMR services, and necessary measures should be taken by health regulatory bodies to increase awareness of HMR and to make use of existing HMR tools among the public. However, further robust research should be conducted to evaluate the effects of HMR programs on reducing hospital admissions and emergency visits.
SUPPLEMENTARY MATERIALS
Supplementary material is available at http://www.e-epih.org/.
epih-41-e2019020-supplementary.pdfNotes
The authors have no conflicts of interest to declare for this study.
Acknowledgements
None.
Notes
AUTHOR CONTRIBUTIONS
Conceptualization: SKG, KKT. Data curation: AK, MC, MR. Formal analysis: SKG, KKT, AK. Funding acquisition: None. Methodology: SKG, AK. Project administration: SKG, AK, KKT. Visualization: MC, MR. Writing – original draft: SKG, AK, KKT. Writing – review & editing: SKG.