Articles
- Page Path
- HOME > Epidemiol Health > Volume 40; 2018 > Article
-
Editorial
Tuberculosis control in the Republic of Korea -
Kyung Sook Cho

-
Epidemiol Health 2018;40:e2018036.
DOI: https://doi.org/10.4178/epih.e2018036
Published online: August 2, 2018
Division of Social Services Projects, Office of Social Welfare Policy, Ministry of Health and Welfare, Sejong, Korea
- Correspondence: Kyung Sook Cho Division of Social Services Projects, Office of Social Welfare Policy, Ministry of Health and Welfare, 13 Doum 4-ro, Sejong 30113, Korea E-mail: ks.g.cho@gmail.com
• Received: May 27, 2018 • Accepted: August 2, 2018
©2018, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- The incidence and mortality rates of tuberculosis (TB) in the Republic of Korea are 77 and 5.2 per 100,000 people, respectively (2016), which are the highest among the member countries of the Organization for Economic Cooperation and Development. Recently, the incidence of TB among teens and individuals in their 20s in the Republic of Korea decreased significantly. The decrease is largely attributed to the TB screening and contact investigation efforts targeting schools over the past few years. However, the incidence of TB among elderly individuals remains high, and it is even increasing compared to that in the past 10 years. Older individuals account for 42% of all TB cases and 82% of TB-related deaths. The success rate of TB treatment in the Republic of Korea has gradually increased due to various programs, such as control of non-compliance, insurance coverage for TB diagnosis and treatment, and TB public–private mix models. This study suggests that policy makers should focus their efforts on policies that prioritize a significant reduction in the incidence of TB based on the 2nd National Strategic Plan for Tuberculosis Control (2018–2022).
- Tuberculosis (TB) has an extremely high global disease burden with more than 10 million new TB cases and approximately 1.7 million TB-related deaths reported annually worldwide [1]. In the Republic of Korea (hereafter Korea), 28,161 new TB cases were reported and the total number of notified patients with TB was 36,044 in 2017. In addition, approximately 2,200 TB-related deaths were reported in 2016 [2].
- Since the initial implementation of the national TB control program in health centers throughout Korea in 1962, the government of Korea has legislated the TB prevention law in 1968 to establish the legal basis for the national TB control program. In 1989, a transition from health center- to private hospital-based TB control program began with the introduction of the nationwide health insurance system, and since 2010, significant effort has focused on TB public–private mix (PPM) model. Recently, TB contact investigation has been reinforced and conducted on family members and other individuals who are in close contact with patients with TB as an effort for the early detection of such condition, and this measure is in addition to the significant effort made in the treatment and management of patients with TB, including free TB diagnosis and treatment and allocation of TB-specialist nurses [3]. Consequently, the prevalence, incidence, and mortality rate associated with TB have steadily decreased over the past few decades. Despite such effort, Korea still had high incidence and mortality rates of TB (77 and 5.2 per 100,000 people, respectively) as of 2016, which represents the highest incidence and mortality rates of TB among all member countries of the Organization for Economic Cooperation and Development (OECD) [1].
- Accordingly, the government of Korea is planning to establish the 2nd National Strategic Plan for Tuberculosis Control (2018–2022) to implement more intensive TB control policies. Thus, the present study aimed to analyze the incidence, prevalence, and mortality rates of TB in Korea as well as the various TB control policies implemented by the government of Korea over the past few decades to present future improvement measures.
INTRODUCTION
- Prevalence, incidence, and mortality rates of tuberculosis
- The mortality rates of TB in Korea were approximately 18.5 and 71.1 per 100,000 population in 1926 and 1942, respectively. However, it increased sharply to 350.0 per 100,000 in 1954 after the Korean War. The mortality rate decreased from 19.7 per 100,000 population in 1983 to 8.9 per 100,000 population in 2000, and as of 2015, the rate is 5.1 per 100,000 population. The incidence rate of TB has decreased by approximately half over a 25-year period (from 168 per 100,000 population in 1990 to 80 per 100,000 population in 2015). The prevalence of TB has also decreased by approximately half (from 940 per 100,000 population in 1965 to 443 per 100,000 population in 1985), and for the following 30 years, the rate decreased to one-quarter of the level to just 101 per 100,000 population in 2015. In particular, the sharp decrease in the prevalence of TB up to 1990 became somewhat sluggish until 2010, and after which, the rate increased sharply again (Figure 1 and Supplementary Material 1).
- Notified tuberculosis cases and deaths
- In Korea, TB has been considered a legal communicable disease since 1957 in accordance with the Infectious Disease Control and Prevention Act, which made its reporting mandatory. In 1968, reporting and registration became mandatory based on the Tuberculosis Prevention Act, whereas the requirement was made more stringent in 2003 with mandatory notification. In 2000, the Tuberculosis Notification Information System was established, requiring all patients with TB to electronically notify and register cases starting in 2001. The total TB cases notified in 2017 were 36,044, representing approximately 22% decrease from 46,082 cases in 2001. The number of new notified TB cases in 2017 was 28,161, representing approximately 21% decrease from 34,123 cases in 2001 [2]. In addition, the rate of total notified TB cases decreased from 96.3 per 100,000 population in 2001 to 70.4 per 100,000 population in 2017. The rate of new notified TB cases also decreased from 71.3 per 100,000 population in 2001 to 55.0 per 100,000 population in 2017, and this showed a decreasing trend in all age groups, except the ≥80-year age group. Compared to other age groups, the 10-19- and 20-29-year age groups showed a more steep decreasing trend, and in particular, the ≤19-year age group showed a decrease to just one-third of the level in 2001 [2,4] (Supplementary Materials 2 and 3). With respect to the total notified TB cases in 2017 based on gender, the percentage of men (60.1%) was significantly higher than that of women (39.9%), whereas the percentage of new notified TB cases was also higher in men (57.3%) than in women (42.7%) [2]. Among the total notified TB cases, the percentage accounted for by elderly individuals aged ≥65 years increased from 20.2% in 2001 to 41.9% in 2017. The number of TB-related mortalities decreased from 3,218 in 2001 to 2,186 in 2016. However, among the total TB-related deaths, the proportion of elderly individuals aged ≥65 years increased from 58.0% in 2001 to 81.7% in 2016 [2] (Supplementary Materials 4).
TUBERCULOSIS IN KOREA
- Changes in the tuberculosis control programs
- Korea began its TB control programs in 1962, focusing on early detection and treatment in health centers located nationwide. Such TB control policy efforts included the following. Starting from 1965, National TB Prevalence Surveys have been conducted every 5 years, and since 2001, Annual reports on the notified TB have been published by notifying and registering all patients with TB in accordance with the Tuberculosis Prevention Act. In 1968, the Tuberculosis Prevention Act was enacted to mark the beginning of a full-fledged implementation of government-led TB control policies. In 2006, the Tuberculosis Elimination Plan by 2030 was established, and in 2013, the National Strategic Plan for Tuberculosis Control was established every 5 years. In particular, the TB PPM model was developed in 2011, and the focus was on the care of patients with TB. That is, TB-specialist nurses were dispatched to 252 health centers and approximately 120 health care facilities throughout Korea. In 2004, TB contact investigation began. By 2009, the budget for TB contact investigation was allocated, and a central epidemiological investigation team has been conducting an official TB contact investigation since 2013. In addition, free government-sponsored TB diagnosis and treatment services are being provided since 2011. In 2017, latent TB infection (LTBI) screening and treatment services were provided to approximately 1.2 million individuals. In 2018, TB screening pilot program for elderly individuals and TB and latent TB screening pilot programs for foreigners were implemented with plans to intensify programs for the vulnerable population that had been neglected until currently (Figure 1). The TB control framework in Korea is shown in Figure 2. Tuberculosis Prevention Act, National Strategic Plan for Tuberculosis Control, and research and development efforts are established based on national TB control policies. Also, various policies and programs are being operated in terms of prevention, early detection, and patient treatment and management (Figure 2).
- Tuberculosis budget
- The budget for national TB control program, which is a national expenditure, increased sharply from 9.9 billion Korean won (KRW) in 2007 to 14.9 billion KRW in 2010 and to 44.7 billion KRW in 2011, and this reflects the fact that government subsidy for personal co-payment amounting to 10% of the health insurance TB treatment cost began in 2011. Such co-payment for TB treatment was waived in 2017, and it is paid in full by health insurance. In 2017, 8.9 billion KRW of relevant budget was paid for the LTBI screening program for healthcare workers, kindergarten teachers, nursery workers, workers in social welfare facilities in accordance with the Tuberculosis Prevention Act, and this accounts for the large margin of increase in expenditure for TB and LTBI early detection programs. However, LTBI screening and treatment was only a 1-year program conducted in 2017 based on the amendment of the law. In 2018, LTBI screening and treatment fees for medical personnel were partially covered, and despite the budgets allocated for new programs in 2018 (620 million KRW for TB screening programs for elderly individuals and 450 million KRW for foreign TB/LTBI screening programs), the total budget was only 34.3 billion KRW (Table 1).
- Tuberculosis prevention
- Despite the high incidence rate of TB in Korea, public interest in and understanding of TB are extremely low. Accordingly, the government of Korea implemented various promotional activities for improving knowledge about TB, encouraging early TB screening, and proper coughing etiquette. In Korea, TB vaccination is mandatory and budget support is provided by the government. The vaccination rate for TB has increased from 16.4% in 1965 to 65.7% in 1990 and from 87.0% in 2003 to 99.8% in 2013 [6,7]. Korea relies solely on imported TB vaccines (bacille de Calmette-Guerin vaccine [BCG] vaccine). However, to resolve the unstable supply of TB vaccines that occurs at certain times and to provide a timely supply of such vaccines, in-country development efforts began in 2014 with 2020 as the target completion date for TB vaccine development (BCG vaccine).
- The prevalence of LTBI is extremely high at 33% in Korea [3,8] (Supplementary Materials 1 and 5). In response to this, prevention is being promoted through LTBI diagnosis and treatment for high-risk groups. For individuals infected with human immunodeficiency virus, TB contacts, organ transplant recipients, tumor necrosis factor users, patients on dialysis, and those with silicosis, who are strongly recommended for systematic LTBI diagnosis and treatment by the World Health Organization (WHO) [9], LTBI screening is provided as medical care benefit under the health insurance [3,10]. Moreover, TB and LTBI screening became mandatory for healthcare workers, postnatal care workers, nursery workers, workers in children welfare facilities, and teachers at kindergartens and primary, secondary, and high schools since 2017 in accordance with the Tuberculosis Prevention Act; the government of Korea paid for systematic LTBI screening and treatment for approximately 1.2 million individuals within this target population [3,10].
- Early detection of tuberculosis
- In Korea, TB screening (chest radiography) is performed as a part of the health examination conducted on children who are entering secondary or high school. For adults, TB screening is included in the health examination performed every 1-2 years for health insurance subscribers. Moreover, the Tuberculosis Prevention Act makes it mandatory for healthcare workers, teachers, nursery workers, and workers in postnatal care centers and children welfare facilities to receive regular TB and LTBI screening. However, the vulnerable population, including elderly individuals, foreigners, and the homeless, have been in the blind spot of TB screening. In response to this, the government of Korea is planning to implement TB screening pilot programs for elderly individuals and TB and LTBI screening pilot programs for foreigners starting in 2018 to establish a systematic early detection strategy for this population.
- Another important aspect of early TB detection is TB contact investigation, and in accordance with the Tuberculosis Prevention Act, TB contact investigation is being conducted on household contacts of TB cases and individuals who are in close contact with patients with TB in schools, hospitals, workplaces, social welfare facilities, armies, and prisons. Beginning with 13 cases in the TB contact investigation in 2004, the number of cases increased to 1,142 in 2013 after the program was fully implemented. Subsequently, the number of cases continued to increase with 1,405, 2,639, and 3,502 cases in 2014, 2015, and 2016, respectively (Supplementary Material 6). In 2016, the number of individuals targeted for TB contact investigation was 146,911, of whom 12,707 were diagnosed with LTBI [11] (Supplementary Material 7).
- Treatment and management of tuberculosis
- In Korea, the notification and registration of all patients with TB are mandatory according to the Tuberculosis Prevention Act. The government is providing diagnosis and treatment services at no cost as well as care until a patient is completely cured. Moreover, the national TB control program also provides financial support for LTBI screening and treatment. Among individuals who were diagnosed with TB in Korea, workers or students are restricted from going to work or school until they are no longer contagious, and they are followed-up to make sure they were under medication for at least 2 weeks. Since 2013, directly observed treatment is being recommended in Korea. However, it still fails to meet the guidelines by the WHO. In addition, treatments for patients who are non-compliant to treatment are being managed through telephone consultation and home visits. The treatment success rates for such non-compliant patients with TB have improved from 56.4% in 2014 to 50.0% in 2015 and to 63.1% in 2016. The total treatment success rate for patients with TB in 2016 was 84.3% for all patients with TB, 86.7% for new patients with TB, and 83.3% for patients with new smear-positive TB. These indicators are showing gradual improvement annually [3].
- Approximately 3.4% of new patients were diagnosed with rifampicin-resistant (RR) and multidrug-resistant (MDR) TB (RR/MDR-TB) in Korea, which is higher than the average of 2.6% among the member countries of the OECD. The repeat patient rate is 11%, which is slightly lower than the average of 12% among the member countries of the OECD [12]. In particular, the percentage of foreigners with MDR-TB in Korea increased from 4.5% in 2011 to 20.5% in 2016 (Supplementary Material 8 and 9). To increase the treatment success rate of patients with MDR-TB in Korea, new high-priced MDR-TB drugs have recently been added to health insurance coverage, and these drugs are being provided at no cost. The treatment success rate of patients with RR/MDR-TB in Korea is 63%, which is similar to the average of 62% among the member countries of the OECD [12].
- One of the most successful models for the treatment and management of patients with TB is the TB PPM model in Korea. After the pilot program in 2007, this model was expanded nationwide in 2011, contributing to the improvements in the treatment success rate for patients with TB through organization cooperation between 252 health centers and approximately 120 general hospitals, wherein 420 TB management specialist nurses have been dispatched to such health centers and hospitals to conduct systematic TB control program, including TB patient consultation, medication guidance, and non-compliant patient management.
TUBERCULOSIS CONTROL IN KOREA
- The incidence and mortality rates of TB in Korea reached their peak after the Korean War in 1950 and subsequently showed a rapid decrease (Figure 1). However, the rates are still the highest among all member countries of the OECD [1,2]. The high incidence of TB in Korea despite its high economic standards may be attributed to the Korean War. The outbreak of TB after a war has been observed in other countries as well [13,14], and a significant portion of the Korean population with poor health conditions, such as malnutrition, dense living environment, and low health care accessibility, may have been infected by LTB after the war [3,5]. The LTBI rate in Korea has decreased steadily from 64.2% in 1960 to 59.3% in 1975, to 44.4% in 1990, and to 33.2% in 2016 (Supplementary Material 5). However, the rate is still higher than that of other advanced countries, such as the US [3,8,15]. The high LTBI rate can be considered as one of the biggest barriers in reducing TB in Korea. In 2017, the government of Korea amended the Tuberculosis Prevention Act to make TB and LTBI screening mandatory for specific groups such as health care and postpartum care workers and teachers. Moreover, systematic LTBI screening and treatment were conducted for 1.2 million individuals [3,10] (Supplementary Material 5 and Supplementary Material 10).
- Recently, the treatment success rate for patients with TB in Korea has improved due to timely diagnosis and treatment. Of which, patient treatment and management based on the TB PPM model have made a significant contribution, leading to a continuous decrease in the incidence of TB [3]. Moreover, a more drastic decrease was observed in the number of patients with TB in the ≤19-year age group than in any other age groups, which may be attributed to the fact that individuals in this age group were born during the period when the incidence of TB was gradually decreasing and full-scale TB contact investigation and TB screening are being conducted at schools [3,4]. However, the incidence of TB among elderly individuals (≥65 years of age) remains high, and the elderly population accounts for 42% of all patients with TB and 82% of all TB-related deaths in Korea. The elderly population shows a lower TB screening rate than the other age groups, and TB control programs for elderly individuals are limited as well. To address such problems, the government of Korea is planning to establish TB control programs for elderly individuals by implementing pilot programs for TB screening and early detection in 2018. By contrast, TB screening is mandatory for foreigners who are from 19 countries with a high incidence rate of TB and enter Korea for residency or work purposes. However, the management of TB among these foreigners after they have entered Korea is difficult. Accordingly, the government of Korea is also planning to launch a pilot program that examines the performance of TB and LTBI screening among foreigners during their stay in Korea.
- The government of Korea established the 2nd National Strategic Plan for Tuberculosis Control (2018–2022) with the goal of lowering the incidence rate of TB from 77 to 40 per 100,000 population by 2022. For the next 5 years, the government of Korea should faithfully execute this plan and allocate the necessary budget according to priorities. First, the top priority for TB control in Korea should be the early diagnosis and treatment of patients with TB. For timely diagnosis and improved treatment rate, health insurance coverage related to TB diagnosis and treatment should be expanded. In addition, to allow timely diagnosis and standardized treatment to be provided at primary care facilities, the reinforcement of the TB PPM program that focuses on medical personnel education and intensive care for patients with TB is also necessary (Supplementary Material 11). Furthermore, research and development efforts for shortening the treatment period and improving the treatment success rate for patients with MDR TB must be expanded. By contrast, measures for the early detection and systematic treatment of TB among the vulnerable population, including elderly individuals, foreigners, and the homeless, who have been neglected until currently, should be explored. With respect to TB treatment for the vulnerable population, a community-based comprehensive public health patient care model should be developed and implemented, whereas greater resources, such as isolation unit for patients with TB and allocation of TB specialist nurses, are also in demand. Second, TB contact investigation should be reinforced to establish an optimal investigation system tailored for collective facilities, such as schools, hospitals, and prisons. The contact investigation should prioritize those in close contact over those in casual contact with individuals with TB, whereas effort is also needed to increase the screening rate for those being tested and treatment success rate for those who tested positive for LTBI [4,12,16-20]. Third, from the TB prevention aspect, promotional strategies must be established for regular TB screening and the timely supply of vaccines by successfully completing the development of TB vaccine that has undergone repeated supply shortage. Moreover, LTBI screening and treatment for high-risk groups including healthcare workers must be continually conducted. Longterm follow-up is needed for LTBI screening and treatment that were performed on 1.2 million individuals in 2017 [12].
DISCUSSION
SUPPLEMENTARY MATERIALS
Figure 1.Annual prevalence, incidence, and mortality rate of tuberculosis (TB). Adapted from Cho KS. Health Soc Welf Rev 2017;37:179-212 [3], with permission of the Korea Institute for Health and Social Affairs.
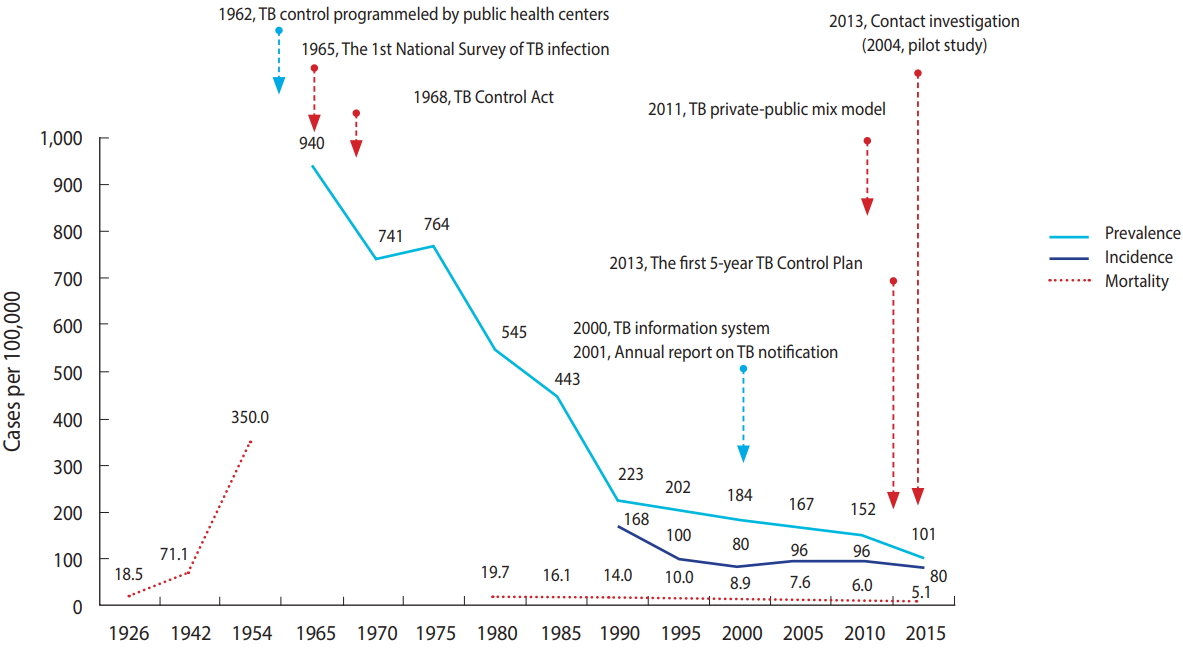
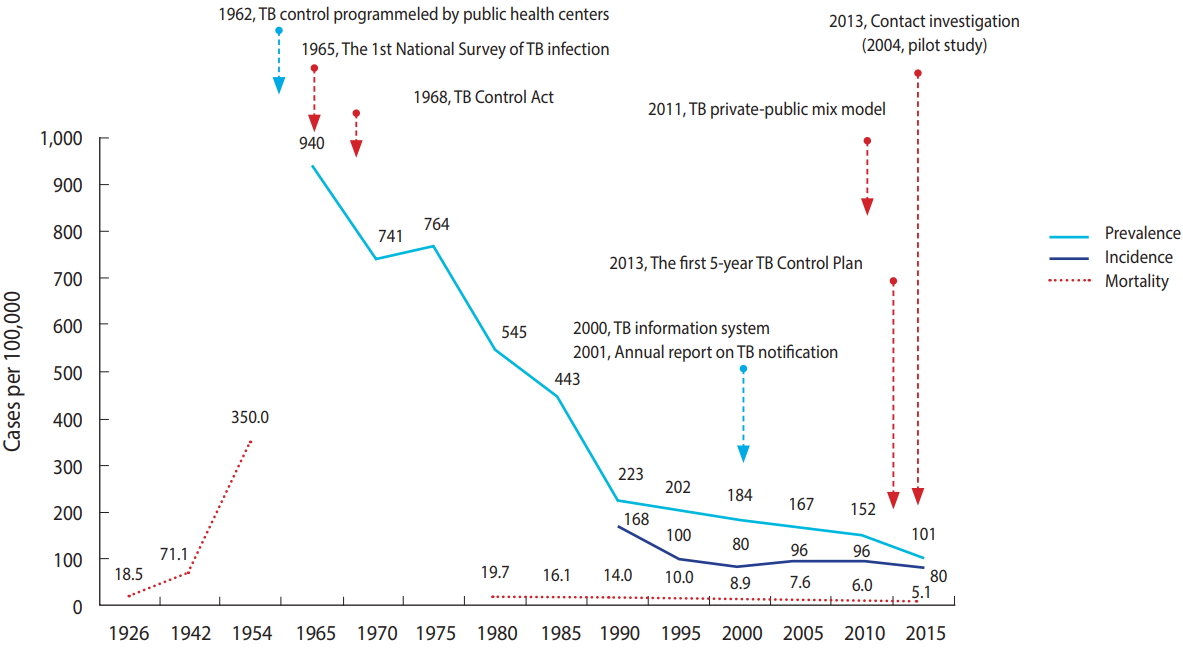
Figure 2.TB control framework of the Republic of Korea. TB, tuberculosis; LTBI, latent TB infection; BCG, bacille de Calmette-Guerin vaccine; PR, public relation; DOT, directly observed treatment; MDR, multidrug-resistant; XDR, extensively drug-registant. Adapted from Cho KS. Health Soc Welf Rev 2017;37:179-212 [3], with permission of the Korea Institute for Health and Social Affairs.
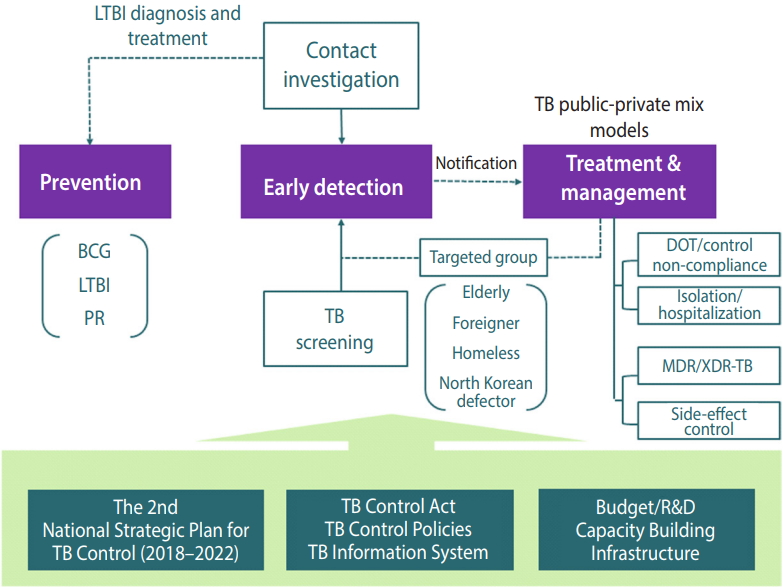
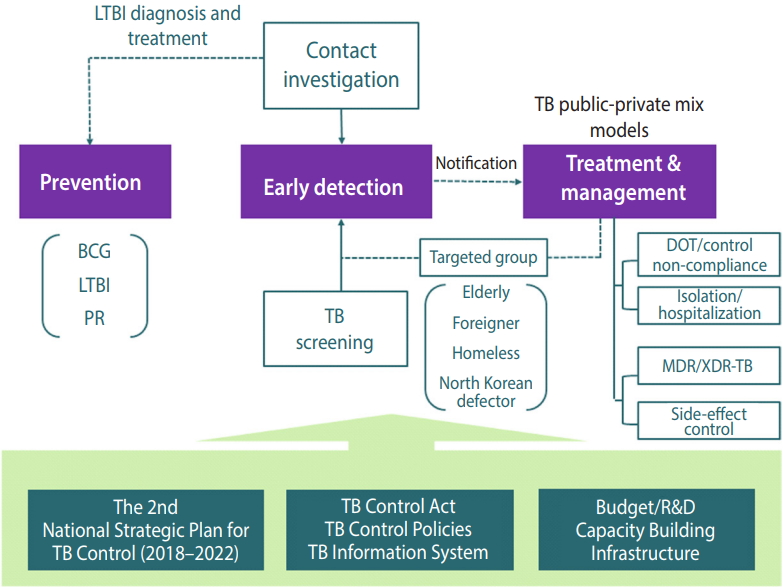
Table 1.TB budgets of central government by year
Unit: 109 Korean won (1,000 Korean won = 1 US dollar).
TB, tuberculosis; LTBI, latent TB infection; NA, not available; R&D, research and development.
Adapted from Cho KS. Health Soc Welf Rev 2017;37:179-212 [3], with permission of the Korea Institute for Health and Social Affairs.
- 1. World Health Organization. Global tuberculosis report 2016; 2016 [cited 2018 Oct 15]. Available from: http://apps.who.int/medicinedocs/en/d/Js23098en/.
- 2. Korea Centers for Disease Control and Prevention. 2017 Annual report on the notified tuberculosis in Korea 2017. Cheongju: Korea Centers for Diseases Control and Prevention; 2018. p 10-52 (Korean).
- 3. Cho KS. Tuberculosis control in the Republic of Korea. Health Soc Welf Rev 2017;37:179-212 (Korean).ArticlePDF
- 4. Cho KS. Tuberculosis incidence and latent tuberculosis infection prevalence in high schools in Korea. Public Health Wkly Rep 2018;11:152-158 (Korean).
- 5. Kim JH, Yim JJ. Achievements in and challenges of tuberculosis control in South Korea. Emerg Infect Dis 2015;21:1913-1920.ArticlePubMedPMC
- 6. Ministry of Health and Welfare. The 7th national tuberculosis prevalence survey. Gwacheon: Ministry of Health and Welfare; 1996. p 9-21 (Korean).
- 7. Lee SG, Jeon SY. National immunization survey 2013. Cheongju: Korea Centers for Diseases Control and Prevention; 2013. p 130 (Korean).
- 8. Korea Centers for Diseases Control and Prevention. 7th Korea National Health and Nutrition Examination Survey 1st year (2016) tuberculin survey support and quality control. Cheongju: Korea Centers for Diseases Control and Prevention; 2016. p 21 (Korean).
- 9. World Health Organization. Guidelines on the management of latent tuberculosis infection; 2015 [cited 2018 Oct 15]. Available from: http://www.who.int/tb/publications/ltbi_document_page/en/.
- 10. Cho KS, Park WS, Jeong HR, Kim MJ, Park SJ, Park AY, et al. Prevalence of latent tuberculosis infection at congregated settings in the Republic of Korea, 2017. Public Health Wkly Rep 2018;11:348-354 (Korean).
- 11. Korea Centers for Diseases Control and Prevention. Report on the contact investigations at congregated settings 2016. Cheongju: Korea Centers for Diseases Control and Prevention; 2017. p 10 (Korean).
- 12. Cho KS, Kim NH. Multidrug-resistant tuberculosis status and performance of the healthcare review committee for new drugs for MDR-TB in the Republic of Korea. Public Health Wkly Rep 2017;10:1362-1368 (Korean).
- 13. Drolet GJ. World War I and tuberculosis. A statistical summary and review. Am J Public Health Nations Health 1945;35:689-697.ArticlePubMedPMC
- 14. Byerly CR; US Borden Institute. Good tuberculosis men: the Army Medical Department’s struggle with tuberculosis. [cited 2018 Oct 15]. Available from: http://www.cs.amedd.army.mil/FileDownloadpublic.aspx?docid=986faf8a-b833-46a8-a251-00f72c91da2f.
- 15. Horsburgh CR Jr, Rubin EJ. Clinical practice. latent tuberculosis infection in the United States. N Engl J Med 2011;364:1441-1448.ArticlePubMed
- 16. Grzybowski S, Barnett GD, Styblo K. Contacts of cases of active pulmonary tuberculosis. Bull Int Union Tuberc 1975;50:90-106.PubMed
- 17. Reichler MR, Reves R, Bur S, Thompson V, Mangura BT, Ford J, et al. Evaluation of investigations conducted to detect and prevent transmission of tuberculosis. JAMA 2002;287:991-995.ArticlePubMed
- 18. Fox GJ, Barry SE, Britton WJ, Marks GB. Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur Respir J 2013;41:140-156.ArticlePubMed
- 19. Sandgren A, Vonk Noordegraaf-Schouten M, van Kessel F, Stuurman A, Oordt-Speets A, van der Werf MJ. Initiation and completion rates for latent tuberculosis infection treatment: a systematic review. BMC Infect Dis 2016;16:204.ArticlePubMedPMCPDF
- 20. Zenner D, Loutet MG, Harris R, Wilson S, Ormerod LP. Evaluating 17 years of latent tuberculosis infection screening in northwest England: a retrospective cohort study of reactivation. Eur Respir J 2017;50:1602505.ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Risk of tuberculosis after endoscopic resection and gastrectomy in gastric cancer: nationwide population-based matched cohort study
Hye Sung Khil, Sue In Choi, Byung-Keun Kim, Eun Joo Lee, Sang Yeub Lee, Ji Hyun Kim, Won Jai Jung
Surgical Endoscopy.2024; 38(3): 1358. CrossRef - Timely Pulmonary Tuberculosis Diagnosis Based on the Epidemiological Disease Spectrum: Population-Based Prospective Cohort Study in the Republic of Korea
Yousang Ko, Jae Seuk Park, Jinsoo Min, Hyung Woo Kim, Hyeon-Kyoung Koo, Jee Youn Oh, Yun-Jeong Jeong, Eunhye Lee, Bumhee Yang, Ju Sang Kim, Sung-Soon Lee, Yunhyung Kwon, Jiyeon Yang, Ji yeon Han, You Jin Jang, Jinseob Kim
JMIR Public Health and Surveillance.2024; 10: e47422. CrossRef - Current Status of Latent Tuberculosis Infection Treatment Among Pediatric Patients in Korea: Prescription and Treatment Completion
Yejin Kim, Kil Seong Bae, Ui Yoon Choi, Seung Beom Han, Jong-Hyun Kim
Journal of Korean Medical Science.2024;[Epub] CrossRef - Safety and outcome of treatment of latent tuberculosis infection in liver transplant recipients
Yun Woo Lee, Hyemin Chung, Sung-Han Kim, Heungsup Sung, Su-Min Ha, Eun-Kyoung Jwa, Dong-Hwan Jung, Deok-Bog Moon, Sung-Gyu Lee, Sang-Oh Lee
Infection.2024; 52(3): 1055. CrossRef - Immunogenicity and protective efficacy of RipA, a peptidoglycan hydrolase, against Mycobacterium tuberculosis Beijing outbreak strains
Kee Woong Kwon, Han-Gyu Choi, Hong-Hee Choi, Eunsol Choi, Hagyu Kim, Hwa-Jung Kim, Sung Jae Shin
Vaccine.2024; 42(8): 1941. CrossRef - Development of a multiplex droplet digital PCR method for detection and monitoring of Mycobacterium tuberculosis and drug-resistant tuberculosis
Yu Jeong Choi, Yoonjung Kim, Hye Jung Park, Dokyun Kim, Hyukmin Lee, Young Ah Kim, Kyung-A Lee
Annals of Clinical Microbiology and Antimicrobials.2024;[Epub] CrossRef - Comparison of active tuberculosis occurrence associated with Janus kinase inhibitors and biological DMARDs in rheumatoid arthritis
Yun-Kyoung Song, Jaehee Lee, Junwoo Jo, Jin-Won Kwon
RMD Open.2024; 10(2): e003946. CrossRef - Drug Persistence and Incidence of Active Tuberculosis of Tumor Necrosis Factor Alpha Inhibitors Versus Tocilizumab as the First-Line Biological Treatment in Patients with Rheumatoid Arthritis: A Nationwide Population-Based Retrospective Cohort Analysis
Min Wook So, A-Ran Kim, Seung-Geun Lee
Rheumatology and Therapy.2024; 11(4): 881. CrossRef - Incidence of Tuberculosis Among Immigrants in Korea Who Participated in a Latent Tuberculosis Infection Screening Program
Yoo Jung Lee, Jinsoo Min, Jun-Pyo Myong, Yun-Hee Lee, Young-Joon Park, Yujin Kim, Gahee Kim, Gyuri Park, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim, Hyung Woo Kim
Journal of Korean Medical Science.2024;[Epub] CrossRef - Socioeconomic disparities and multidrug-resistant tuberculosis in South Korea: Focus on immigrants and income levels
Han Eol Jeong, Sungho Bea, Ju Hwan Kim, Seung Hun Jang, Hyunjin Son, Ju-Young Shin
Journal of Microbiology, Immunology and Infection.2023; 56(2): 424. CrossRef - Tuberculosis and the Risk of Ischemic Heart Disease: A Nationwide Cohort Study
Han Rim Lee, Jung Eun Yoo, Hayoung Choi, Kyungdo Han, Young-Hyo Lim, Hyun Lee, Dong Wook Shin
Clinical Infectious Diseases.2023; 76(9): 1576. CrossRef - A prospective patient registry to monitor safety, effectiveness, and utilisation of bedaquiline in patients with multidrug-resistant tuberculosis in South Korea
Tae Sun Shim, Helen Pai, JeongHa Mok, Seung Heon Lee, Yong-Soo Kwon, Jae Chol Choi, JaeSeok Park, Eileen Birmingham, Gary Mao, Lori Alquier, Kourtney Davis, Florence Thoret-Bauchet, Ji Hyun Kim, Hyeongyeong Kim, Nyasha Bakare
BMC Infectious Diseases.2023;[Epub] CrossRef - Predictive Factors and Clinical Impacts of Delayed Isolation of Tuberculosis during Hospital Admission
Inhan Lee, Soyoung Kang, Bumsik Chin, Joon-Sung Joh, Ina Jeong, Junghyun Kim, Joohae Kim, Ji Yeon Lee
Journal of Clinical Medicine.2023; 12(4): 1361. CrossRef - Tuberculosis in older adults: case studies from four countries with rapidly ageing populations in the western pacific region
Alvin Kuo Jing Teo, Kalpeshsinh Rahevar, Fukushi Morishita, Alicia Ang, Takashi Yoshiyama, Akihiro Ohkado, Lisa Kawatsu, Norio Yamada, Kazuhiro Uchimura, Youngeun Choi, Zi Chen, Siyan Yi, Manami Yanagawa, Kyung Hyun Oh, Kerri Viney, Ben Marais, Heejin Kim
BMC Public Health.2023;[Epub] CrossRef - Cost-Effectiveness of All-Oral Regimens for the Treatment of Multidrug-Resistant Tuberculosis in Korea: Comparison With Conventional Injectable-Containing Regimens
Hae-Young Park, Jin-Won Kwon, Hye-Lin Kim, Sun-Hong Kwon, Jin Hyun Nam, Serim Min, In-Sun Oh, Sungho Bea, Sun Ha Choi
Journal of Korean Medical Science.2023;[Epub] CrossRef - A comparison of phenotypic and WGS drug susceptibility testing in Mycobacterium tuberculosis isolates from the Republic of Korea
Seung Heon Lee, Elena Ferran, Adam A Witney, Sungweon Ryu, Hyungseok Kang, Nathaniel Storey, Timothy D McHugh, Giovanni Satta
JAC-Antimicrobial Resistance.2023;[Epub] CrossRef - Comparative safety of bedaquiline and delamanid in patients with multidrug resistant tuberculosis: A nationwide retrospective cohort study
Ju Hwan Kim, Hyesung Lee, In-Sun Oh, Han Eol Jeong, Sungho Bea, Seung Hun Jang, Hyunjin Son, Ju-Young Shin
Journal of Microbiology, Immunology and Infection.2023; 56(4): 842. CrossRef - Development of a population pharmacokinetic model of pyrazinamide to guide personalized therapy: impacts of geriatric and diabetes mellitus on clearance
Ryunha Kim, Rannissa Puspita Jayanti, Hongyeul Lee, Hyun-Kuk Kim, Jiyeon Kang, I-Nae Park, Jehun Kim, Jee Youn Oh, Hyung Woo Kim, Heayon Lee, Jong-Lyul Ghim, Sangzin Ahn, Nguyen Phuoc Long, Yong-Soon Cho, Jae-Gook Shin, On behalf of the cPMTb
Frontiers in Pharmacology.2023;[Epub] CrossRef - Factor analysis of the role of physicians and its associated factors for encompassing patients with suspected tuberculosis in Surabaya City
Rosita D. Yuliandari, Chatarina Umbul Wahyuni, Fariani Syahrul, Hari B. Notobroto, Mochammad B. Qomaruddin, Soedarsono Soedarsono
Journal of Public Health in Africa.2023; 14(2): 5. CrossRef - Risk of mortality and clinical outcomes associated with healthcare delay among patients with tuberculosis
Sungho Bea, Hyesung Lee, Won Suk Choi, Kyungmin Huh, Jaehun Jung, Ju-Young Shin
Journal of Infection and Public Health.2023; 16(8): 1313. CrossRef - Research Progress of Information Technology Applied to the Management of Pulmonary Tuberculosis Patients
曼丽 舒
Advances in Clinical Medicine.2023; 13(06): 8871. CrossRef - Incidence and treatment trends of infectious spondylodiscitis in South Korea: A nationwide population-based study
Hee Jung Son, Myongwhan Kim, Dong Hong Kim, Chang-Nam Kang, Hiroshi Hashizume
PLOS ONE.2023; 18(6): e0287846. CrossRef - Institutional Tuberculosis Control and Elimination Program
Shi Nae Yu, Tae Hyong Kim, Su Ha Han, Yang-Ki Kim
Korean Journal of Healthcare-Associated Infection Control and Prevention.2023; 28(1): 22. CrossRef - Comparison of the Standard E TB-Feron ELISA and QuantiFERON-TB Gold PLUS assays: the advantageous use of whole recombinant protein antigens for latent tuberculosis diagnosis
Da-Gyum Lee, Jihye Kang, Jihee Jung, Taeyoon Kim, Jiyeon Kim, Hyunjin Lee, Junghee Lee, Youngsub Won, Sungweon Ryoo
Letters in Applied Microbiology.2023;[Epub] CrossRef - Risk of loss to follow-up among tuberculosis patients in South Korea: whom should we focus on?
Hyung Woo Kim, Jinsoo Min, Yousang Ko, Jee Youn Oh, Yun-Jeong Jeong, Eun Hye Lee, Bumhee Yang, Hyeon-Kyoung Koo, Sung-Soon Lee, Jae Seuk Park, Kwang Joo Park, Jung Hyun Chang, Joonsung Joh, Min Ki Lee, Ju Sang Kim
Frontiers in Public Health.2023;[Epub] CrossRef - Risk adjustment model for tuberculosis compared to non-tuberculosis mycobacterium or latent tuberculosis infection: Center for Personalized Precision Medicine of Tuberculosis (cPMTb) cohort database
Woo Jung Seo, Hyeon-Kyoung Koo, Ji Yeon Kang, Jieun Kang, So Hee Park, Hyung Koo Kang, Hye Kyeong Park, Sung-Soon Lee, Sangbong Choi, Tae Won Jang, Kyeong-Cheol Shin, Jee Youn Oh, Joon Young Choi, Jinsoo Min, Young-Kyung Choi, Jae-Gook Shin, Yong-Soon Cho
BMC Pulmonary Medicine.2023;[Epub] CrossRef - Cohort Profile: Gachon Regional Occupational Cohort Study (GROCS)
Wanhyung Lee, Yongho Lee, Junhyeong Lee, Uijin Kim, Eunsun Han, Seunghon Ham, Won-Jun Choi, Seong-Kyu Kang
Safety and Health at Work.2022; 13(1): 112. CrossRef - Factors Related to Successful Tuberculosis Treatment in Vulnerable Groups
Younghyun Kim, Ji Yeon Lee, Ina Jeong, Junghyun Kim, Joohae Kim, Jiyeon Han, Eunjin Jeong, Ah Yeon Han, Joon-Sung Joh, Jung-Duck Park
The Korean Journal of Medicine.2022; 97(1): 50. CrossRef - Comparison of Disability-Adjusted Life Years (DALYs) and Economic Burden on People With Drug-Susceptible Tuberculosis and Multidrug-Resistant Tuberculosis in Korea
SeungCheor Lee, Moon Jung Kim, Seung Heon Lee, Hae-Young Kim, Hee-Sun Kim, In-Hwan Oh
Frontiers in Public Health.2022;[Epub] CrossRef - Four months of rifampicin monotherapy for latent tuberculosis infection in children
Chi Eun Oh, Dick Menzies
Clinical and Experimental Pediatrics.2022; 65(5): 214. CrossRef - Skin manifestations and clinical features of drug reaction with eosinophilia and systemic symptoms: a retrospective multicentre study of 125 patients
J.W. Lee, S.R. Lee, M.J. Kim, S. Cho, S.W. Youn, M.S. Yang, S.H. Kim, H.R. Kang, O. Kwon
Journal of the European Academy of Dermatology and Venereology.2022; 36(9): 1584. CrossRef - Relational Agents for the Homeless with Tuberculosis Experience
Yi Hyun Jang, Soo Han Im, Younah Kang, Joon Sang Baek
ACM Transactions on Interactive Intelligent Systems.2022;[Epub] CrossRef - Cohort Profile: Korean Tuberculosis and Post-Tuberculosis Cohort Constructed by Linking the Korean National Tuberculosis Surveillance System and National Health Information Database
Dawoon Jeong, Hee-Yeon Kang, Jinsun Kim, Hyewon Lee, Bit-Na Yoo, Hee-Sun Kim, Hongjo Choi
Journal of Preventive Medicine and Public Health.2022; 55(3): 253. CrossRef - Comparison of developing tuberculosis following tumor necrosis factor inhibition and interleukin-6 inhibition in patients with rheumatoid arthritis: a nationwide observational study in South Korea, 2013–2018
Seung Min Jung, Minkyung Han, Eun Hwa Kim, Inkyung Jung, Yong-Beom Park
Arthritis Research & Therapy.2022;[Epub] CrossRef - High Procalcitonin, C-Reactive Protein, and α-1 Acid Glycoprotein Levels in Whole Blood Samples Could Help Rapid Discrimination of Active Tuberculosis from Latent Tuberculosis Infection and Healthy Individuals
Yun-Jeong Kang, Heechul Park, Sung-Bae Park, Jiyoung Lee, Hyanglan Hyun, Minju Jung, Eun Ju Lee, Min-A Je, Jungho Kim, Yong Sung Lee, Sunghyun Kim
Microorganisms.2022; 10(10): 1928. CrossRef - Incidence, risk factors, and final causes for misdiagnosis of tuberculosis in the Republic of Korea: a population-based longitudinal analysis
Changwhan Kim, Yousang Ko, Jin-Wook Moon, Yong-Bum Park, So Young Park, Ga-Young Ban, Ju Yeun Song, Hajeong Kim, Yun Su Sim, Ji Young Park, Chang Youl Lee
European Respiratory Journal.2022; 60(4): 2201461. CrossRef - Tuberculosis and Risk of Ischemic Stroke: A Nationwide Cohort Study
Han Rim Lee, Jung Eun Yoo, Hayoung Choi, Kyungdo Han, Jin Hyung Jung, Jongkyu Park, Hyun Lee, Dong Wook Shin
Stroke.2022; 53(11): 3401. CrossRef - Fatal Pneumonia Caused by Omicron Subvariant BA.2 of Severe Acute Respiratory Syndrome Coronavirus 2 with the Pulmonary Tuberculosis
Jin-Haeng Heo, Young-Il Park, Young San Ko, Ho Suk Song, Suk Hoon Ham, Hoon Kwon, Joo-Young Na
Korean Journal of Legal Medicine.2022; 46(3): 79. CrossRef - Renal Hydatid With Tuberculosis in a Child: A Rare Coexistence
Sravanthi Vutukuru, Shailesh Solanki, Prema Menon, Nitin Peters, Ram Samujh, Radhika Srinivasan
Advances in Pediatric Surgery.2022; 28(2): 76. CrossRef - The Rise in Prevalence and Related Costs of Nontuberculous Mycobacterial Diseases in South Korea, 2010–2021
Joong-Yub Kim, Nakwon Kwak, Jae-Joon Yim
Open Forum Infectious Diseases.2022;[Epub] CrossRef - Evaluation of the accessibility and its equity of the national public-private mix (PPM) program for tuberculosis in South Korea: a multilevel analysis
Hyunjin Son, Changhoon Kim
Epidemiology and Health.2022; : e2023002. CrossRef - Estimating the burden of nosocomial exposure to tuberculosis in South Korea, a nationwide population based cross-sectional study
Hyung Woo Kim, Jun-Pyo Myong, Ju Sang Kim
The Korean Journal of Internal Medicine.2021; 36(5): 1134. CrossRef - Treatment Outcomes of Patients with Multidrug-Resistant Tuberculosis: Comparison of Pre- and Post-Public–Private Mix Periods
Yewon Kang, Eun-Jung Jo, Jung Seop Eom, Mi-Hyun Kim, Kwangha Lee, Ki Uk Kim, Hye-Kyung Park, Min Ki Lee, Jeongha Mok
Tuberculosis and Respiratory Diseases.2021; 84(1): 74. CrossRef - Easily accessed nitroquinolones exhibiting potent and selective anti-tubercular activity
Phelelisiwe S. Dube, Lesetja J. Legoabe, Audrey Jordaan, Omobolanle J. Jesumoroti, Tendamudzimu Tshiwawa, Digby F. Warner, Richard M. Beteck
European Journal of Medicinal Chemistry.2021; 213: 113207. CrossRef - Clinical and radiologic characteristics of radiologically missed miliary tuberculosis
Jooae Choe, Kyung Hwa Jung, Joung-Ha Park, Sung-Han Kim, Mi Young Kim
Medicine.2021; 100(8): e23833. CrossRef - Screening for Mycobacterium tuberculosis Infection Using Beijing/K Strain-Specific Peptides in a School Outbreak Cohort
Ji Young Hong, Ahreum Kim, So Yeong Park, Sang-Nae Cho, Hazel M. Dockrell, Yun-Gyoung Hur
Frontiers in Cellular and Infection Microbiology.2021;[Epub] CrossRef - Age-Specific Mathematical Model for Tuberculosis Transmission Dynamics in South Korea
Sunmi Lee, Hae-Young Park, Hohyung Ryu, Jin-Won Kwon
Mathematics.2021; 9(8): 804. CrossRef - Health-Related Quality of Life Based on EQ-5D Utility Score in Patients With Tuberculosis: A Systematic Review
Hae-Young Park, Hyo-Bin Cheon, Sun Ha Choi, Jin-Won Kwon
Frontiers in Pharmacology.2021;[Epub] CrossRef - Current situation of tuberculosis and National Strategic Plan for Tuberculosis Control in Korea
Eunjeong Son, Doosoo Jeon
Journal of the Korean Medical Association.2021; 64(4): 316. CrossRef - Anemia, sarcopenia, physical activity, and the risk of tuberculosis in the older population: a nationwide cohort study
Jung Eun Yoo, Dahye Kim, Hayoung Choi, Young Ae Kang, Kyungdo Han, Hyun Lee, Dong Wook Shin
Therapeutic Advances in Chronic Disease.2021; 12: 204062232110159. CrossRef - Incidence of tuberculosis in advanced lung cancer patients treated with immune checkpoint inhibitors – A nationwide population-based cohort study
Hyung Woo Kim, Ju Sang Kim, Sang Haak Lee
Lung Cancer.2021; 158: 107. CrossRef - Combined analysis of whole blood interferon gamma release assay and complete blood count analysis for rapid discrimination of active tuberculosis and latent tuberculosis infection
Yun-Jeong Kang, Heechul Park, Sung-Bae Park, Junseong Kim, Jiyoung Lee, Jungho Kim, Sunyoung Park, Yong Sung Lee, Sunghyun Kim
Journal of Clinical Tuberculosis and Other Mycobacterial Diseases.2021; 24: 100253. CrossRef - Delayed Diagnosis of Tuberculosis Mistaken for Tinea Corporis in a Healthy Adult
Jae-Wang Kim, Jeong Rae Yoo, Hyunjoo Oh, Misun Kim, Sang Taek Heo
Tuberculosis and Respiratory Diseases.2021; 84(3): 245. CrossRef - Effect of serum isoniazid level on treatment outcomes among tuberculosis patients with slow response – A retrospective cohort study
Hyung Woo Kim, Ah Young Shin, Jick Hwan Ha, Joong Hyun Ahn, Hye Seon Kang, Ju Sang Kim
Journal of Infection and Chemotherapy.2021; 27(11): 1555. CrossRef - TB Antigen-Stimulated CXCR3 Ligand Assay for Diagnosis of Tuberculous Lymphadenitis
Wou-Young Chung, Keu-Sung Lee, Joo-Hun Park, Yun-Jung Jung, Seung-Soo Sheen, Ji-Eun Park, Joo-Sung Sun, Young-Hwa Ko, Kwang-Joo Park
International Journal of Environmental Research and Public Health.2021; 18(15): 8020. CrossRef - A 10-Year Single-Center Experience of Adverse Drug Reaction Monitoring
Soo Been Park, Mira Moon, Hyun Hwa Kim, Ga-Yoon Park, Dong Yoon Kang, Ju-Yeun Lee, Yoon Sook Cho, Hye-Ryun Kang, Sang-Heon Cho
The Korean Journal of Medicine.2021; 96(4): 341. CrossRef - Health-related quality of life after pulmonary tuberculosis in South Korea: analysis from the Korea National Health and Nutrition Examination Survey between 2010 and 2018
Sang Hyuk Kim, Hyun Lee, Youlim Kim
Health and Quality of Life Outcomes.2021;[Epub] CrossRef - Pulmonary mycobacterial infection is associated with increased mortality in patients with acute respiratory distress syndrome
Jong Hwan Jeong, Manbong Heo, Sunmi Ju, Seung Jun Lee, Yu Ji Cho, Yi Yeong Jeong, Jong Deog Lee, Jung-Wan Yoo
Medicine.2021; 100(33): e26969. CrossRef - The cumulative dose-dependent effects of metformin on the development of tuberculosis in patients newly diagnosed with type 2 diabetes mellitus
Eunyoung Heo, Eunyoung Kim, Eun Jin Jang, Chang-Hoon Lee
BMC Pulmonary Medicine.2021;[Epub] CrossRef - The Relationship Between Socio-Demographic Factors and Tuberculosis Mortality in the Republic of Korea During 2008–2017
SeoYeon Chung, Jeong-Yeon Seon, Seung Heon Lee, Hae-Young Kim, Yeo Wool Lee, Kyoungeun Bae, In-Hwan Oh
Frontiers in Public Health.2021;[Epub] CrossRef - Clinical Factors Associated with Cavitary Tuberculosis and Its Treatment Outcomes
Sun-Hyung Kim, Yoon Mi Shin, Jin Young Yoo, Jun Yeun Cho, Hyeran Kang, Hyun Lee, Kang Hyeon Choe, Ki Man Lee, Bumhee Yang
Journal of Personalized Medicine.2021; 11(11): 1081. CrossRef - Decreased annual risk of tuberculosis infection in South Korean healthcare workers using interferon-gamma release assay between 1986 and 2005
Eun Hye Lee, Nak-Hoon Son, Se Hyun Kwak, Ji Soo Choi, Min Chul Kim, Chang Hwan Seol, Sung-Ryeol Kim, Byung Hoon Park, Young Ae Kang
BMC Infectious Diseases.2021;[Epub] CrossRef - Risk Groups of Developing Active Tuberculosis in Liver Transplant Recipients in a Tuberculosis Endemic Area: Risk Stratification by Chest Image and Interferon Gamma Release Assay
Si-Ho Kim, Suhyun Oh, Eliel Nham, Jae-Hoon Ko, Kyungmin Huh, Sun Young Cho, Cheol-In Kang, Doo Ryeon Chung, Gyu-Seong Choi, Jong Man Kim, Jae-Won Joh, Kyong Ran Peck
International Journal of Infectious Diseases.2021; 113: 359. CrossRef - Incidence rate of active tuberculosis in solid organ transplant recipients: Data from a nationwide population cohort in a high‐endemic country
Da Eun Kwon, Sang Hoon Han, Kyung Do Han, Yeonju La, Kyoung Hwa Lee
Transplant Infectious Disease.2021;[Epub] CrossRef - Treatment of Isoniazid-Resistant Pulmonary Tuberculosis
Byung Woo Jhun, Won-Jung Koh
Tuberculosis and Respiratory Diseases.2020; 83(1): 20. CrossRef - Development of tuberculosis in cancer patients receiving immune checkpoint inhibitors
Yunjoo Im, Jeeyun Lee, Seok Jin Kim, Won-Jung Koh, Byung Woo Jhun, Se-Hoon Lee
Respiratory Medicine.2020; 161: 105853. CrossRef - One Step toward a Low Tuberculosis-Burden Country: Screening for Tuberculosis Infection among the Immigrants and Refugees
Hyung Woo Kim, Ju Sang Kim
Tuberculosis and Respiratory Diseases.2020; 83(1): 104. CrossRef - Changes in the medical burden of pyogenic and tuberculous spondylitis between 2007 and 2016: A nationwide cohort study
Yeo Song Kim, Jeong Gyun Kim, Jeeeun Yi, Jung Min Choi, Chun Kee Chung, Un Yong Choi, In-bo Han, Seil Sohn
Journal of Clinical Neuroscience.2020; 73: 89. CrossRef - The use of biological disease-modifying antirheumatic drugs for inflammatory arthritis in Korea: results of a Korean Expert Consensus
Eun-Jung Park, Hyungjin Kim, Seung Min Jung, Yoon-Kyoung Sung, Han Joo Baek, Jisoo Lee
The Korean Journal of Internal Medicine.2020; 35(1): 41. CrossRef - The Use of Biological Disease-modifying Antirheumatic Drugs for Inflammatory Arthritis in Korea: Results of a Korean Expert Consensus
Eun-Jung Park, Hyungjin Kim, Seung Min Jung, Yoon-Kyoung Sung, Han Joo Baek, Jisoo Lee
Journal of Rheumatic Diseases.2020; 27(1): 4. CrossRef - Risk factors of delayed isolation of patients with pulmonary tuberculosis
C.-J. Kim, Y. Kim, J.Y. Bae, A. Kim, J. Kim, H.J. Son, H.J. Choi
Clinical Microbiology and Infection.2020; 26(8): 1058. CrossRef - Ustekinumab does not increase tuberculosis risk: Results from a national database in South Korea
Soo Ick Cho, Sungchan Kang, Ye Eun Kim, Jin Yong Lee, Seong Jin Jo
Journal of the American Academy of Dermatology.2020; 82(5): 1243. CrossRef - Latent tuberculosis infection: recent progress and challenges in South Korea
Doosoo Jeon
The Korean Journal of Internal Medicine.2020; 35(2): 269. CrossRef - Early discontinuation of tofacitinib in patients with rheumatoid arthritis co-treated with rifampin for latent tuberculosis
So Hye Nam, Ji Seon Oh, Seokchan Hong, Tae Sun Shim, Chang-Keun Lee, Bin Yoo, Yong-Gil Kim
Joint Bone Spine.2020; 87(5): 475. CrossRef - Optimizing hospital distribution across districts to reduce tuberculosis fatalities
Mi Jin Lee, Kanghun Kim, Junik Son, Deok-Sun Lee
Scientific Reports.2020;[Epub] CrossRef - Correction: “Changes in the medical burden of pyogenic and tuberculous spondylitis between 2007 and 2016: A nationwide cohort study”
Yeo Song Kim, Jeong Gyun Kim, Jeeeun Yi, Jung Min Choi, Chun Kee Chung, Un Yong Choi, In-bo Han, Seil Sohn
Journal of Clinical Neuroscience.2020; 78: 347. CrossRef - Trends in long-term glucocorticoid use and risk of 5-year mortality: a historical cohort study in South Korea
Tak Kyu Oh, In-Ae Song
Endocrine.2020; 69(3): 634. CrossRef - Self-care Efficacy and Health-related Quality of Life among Patients on Primary Treatment for Pulmonary Tuberculosis: The Mediating Effects of Self-Care Performance
Hyun Ju Lee, Jiyoung Park
Korean Journal of Adult Nursing.2020; 32(3): 305. CrossRef - Tuberculosis Surveillance and Monitoring under the National Public-Private Mix Tuberculosis Control Project in South Korea 2016–2017
Jinsoo Min, Hyung Woo Kim, Yousang Ko, Jee Youn Oh, Ji Young Kang, Joosun Lee, Young Joon Park, Sung-Soon Lee, Jae Seuk Park, Ju Sang Kim
Tuberculosis and Respiratory Diseases.2020; 83(3): 218. CrossRef - A review of the designated health care institution for child abuse in Korea and the compatible systems in other countries
Myung Hun Kim, Young Ho Kwak
Pediatric Emergency Medicine Journal.2020; 7(1): 1. CrossRef - Estimating Disability-Adjusted Life Years due to Tuberculosis in Korea through to the Year 2040
Su Yeon Jang, Moon Jung Kim, Hyeon-Kyoung Cheong, In-Hwan Oh
International Journal of Environmental Research and Public Health.2020; 17(16): 5960. CrossRef - Replicated Association Study between Tuberculosis and CLCN6, DOK7, HLA-DRA in Korean
Sung-Soo Kim, Min Park, Sangjung Park
Biomedical Science Letters.2020; 26(3): 238. CrossRef - Incidence of bronchiectasis concerning tuberculosis epidemiology and other ecological factors: A Korean National Cohort Study
Hayoung Choi, Jiin Ryu, Youlim Kim, Bumhee Yang, Bin Hwangbo, Sun-Young Kong, Yun Su Sim, Hye Yun Park, Seung Won Ra, Yeon-Mok Oh, Ji-Yong Moon, Tae-Hyung Kim, Sang-Heon Kim, Jang Won Sohn, Ho Joo Yoon, Hyun Lee
ERJ Open Research.2020; 6(4): 00097-2020. CrossRef - Incidence of Tuberculosis in Systemic Necrotizing Vasculitides: A Population-Based Study From an Intermediate-Burden Country
Sung Soo Ahn, Minkyung Han, Juyoung Yoo, Yong-Beom Park, Inkyung Jung, Sang-Won Lee
Frontiers in Medicine.2020;[Epub] CrossRef - Higher risk of tuberculosis in combination therapy for inflammatory bowel disease
Seong Ji Choi, Min Sun Kim, Eun Sun Kim, Juneyoung Lee, Jae Min Lee, Hyuk Soon Choi, Bora Keum, Yoon Tae Jeen, Hong Sik Lee, Hoon Jai Chun, Chang Duck Kim
Medicine.2020; 99(44): e22897. CrossRef - Clinical profiles of subclinical disease among pulmonary tuberculosis patients: a prospective cohort study in South Korea
Jinsoo Min, Chaeuk Chung, Sung Soo Jung, Hye Kyeong Park, Sung-Soon Lee, Ki Man Lee
BMC Pulmonary Medicine.2020;[Epub] CrossRef - Risk-benefit analysis of isoniazid monotherapy to prevent tuberculosis in patients with rheumatic diseases exposed to prolonged, high-dose glucocorticoids
Jun Won Park, Jeffrey R. Curtis, Hajeong Lee, Jung-Kyu Lee, Yeong Wook Song, Eun Bong Lee, Frederick Quinn
PLOS ONE.2020; 15(12): e0244239. CrossRef - Clinical Analysis of Laryngeal Tuberculosis: Recent 10 Years’ Experience in a Single Institution
Ji-Hoon Kim, Tae Hoon Kong, Hong-Shik Choi, Hyung Kwon Byeon
Journal of The Korean Society of Laryngology, Phoniatrics and Logopedics.2020; 31(2): 61. CrossRef - Notified Incidence of Tuberculosis in Foreign-born Individuals in Jeju Province, Republic of Korea
Dae Soon Kim, Jong-Myon Bae
Journal of Preventive Medicine and Public Health.2019; 52(1): 66. CrossRef - Factors Influencing the Diagnosis and Treatment of Latent Tuberculosis among Contacts in Congregated Settings in Korea
Ahreum Kim, Minhyeok Choi
Journal of Korean Medical Science.2019;[Epub] CrossRef - Experiences of Latent Tuberculosis Infection Treatment for the North Korean Refugees
Beong Ki Kim, Hee Jin Kim, Ho Jin Kim, Jae Hyung Cha, Jin Beom Lee, Jeonghe Jeon, Chi Young Kim, Young Kim, Je Hyeong Kim, Chol Shin, Seung Heon Lee
Tuberculosis and Respiratory Diseases.2019; 82(4): 306. CrossRef - Active Case Finding in the Elderly Tuberculosis in South Korea
Seung Heon Lee
Tuberculosis and Respiratory Diseases.2019; 82(3): 261. CrossRef - Research Areas and Trends in Articles on Pediatric and Adolescent Tuberculosis in Korea
Ho Yoon Lim, Jung Hyun Lee, Yu Jin Jung, Chi Eun Oh
Pediatric Infection & Vaccine.2019; 26(2): 89. CrossRef - Clinical profiles of early and tuberculosis-related mortality in South Korea between 2015 and 2017: a cross-sectional study
Jinsoo Min, Ju Sang Kim, Hyung Woo Kim, Ah Young Shin, Hyeon-Kyoung Koo, Sung-Soon Lee, Yang-Ki Kim, Kyeong-Cheol Shin, Jung Hyun Chang, Gayoung Chun, Joosun Lee, Mi Sun Park, Jae Seuk Park
BMC Infectious Diseases.2019;[Epub] CrossRef - Completion rate of latent tuberculosis infection treatment in patients aged 65 years and older
Chang Suk Noh, Hwan Il Kim, Hayoung Choi, Youlim Kim, Cheol-Hong Kim, Jeong-Hee Choi, In Gyu Hyun, Moon Seong Baek
Respiratory Medicine.2019; 157: 52. CrossRef - Evaluation and treatment of latent tuberculosis infection among healthcare workers in Korea: A multicentre cohort analysis
Seon-Sook Han, Su Jin Lee, Jae-Joon Yim, Jin Hwa Song, Eun Hye Lee, Young Ae Kang, Lei Gao
PLOS ONE.2019; 14(9): e0222810. CrossRef - Nutritional Adequacy and Latent Tuberculosis Infection in End-Stage Renal Disease Patients
Seung Don Baek, Soomin Jeung, Jae-Young Kang
Nutrients.2019; 11(10): 2299. CrossRef - Screening and Treatment of Latent Tuberculosis Infection among Healthcare Workers at a Referral Hospital in Korea
Se Yoon Park, Eunyoung Lee, Eun Jung Lee, Tae Hyong Kim, Yang-Ki Kim
Infection & Chemotherapy.2019; 51(4): 355. CrossRef - Tuberculosis control in the Republic of Korea
Kyung Sook Cho
Epidemiology and Health.2018; 40: e2018036. CrossRef

 KSE
KSE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite



