Articles
- Page Path
- HOME > Epidemiol Health > Volume 45; 2023 > Article
-
COVID-19
Brief Communication
Clinical severity according to the primary infection variant in patients with suspected SARS-CoV-2 reinfection in Korea -
Myung-Jae Hwang1*
 , Insob Hwang1*
, Insob Hwang1* , Chungmin Park1
, Chungmin Park1 , Hanul Park1
, Hanul Park1 , Taejong Son1
, Taejong Son1 , Jong-Hun Kim2
, Jong-Hun Kim2
-
Epidemiol Health 2022;45:e2023007.
DOI: https://doi.org/10.4178/epih.e2023007
Published online: December 21, 2022
1Division of Infectious Disease Response, Gyeongbuk Regional Center for Disease Control and Prevention, Korea Disease Control and Prevention Agency, Daegu, Korea
2Department of Social and Preventive Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea
- Correspondence: Jong-Hun Kim Department of Social and Preventive Medicine, Sungkyunkwan University School of Medicine, 2066 Seobu-ro, Jangan-gu, Suwon 16419, Korea E-mail: kimjh32@skku.edu
- *Hwang & Hwang contributed equally to this work as joint first authors.
© 2023, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
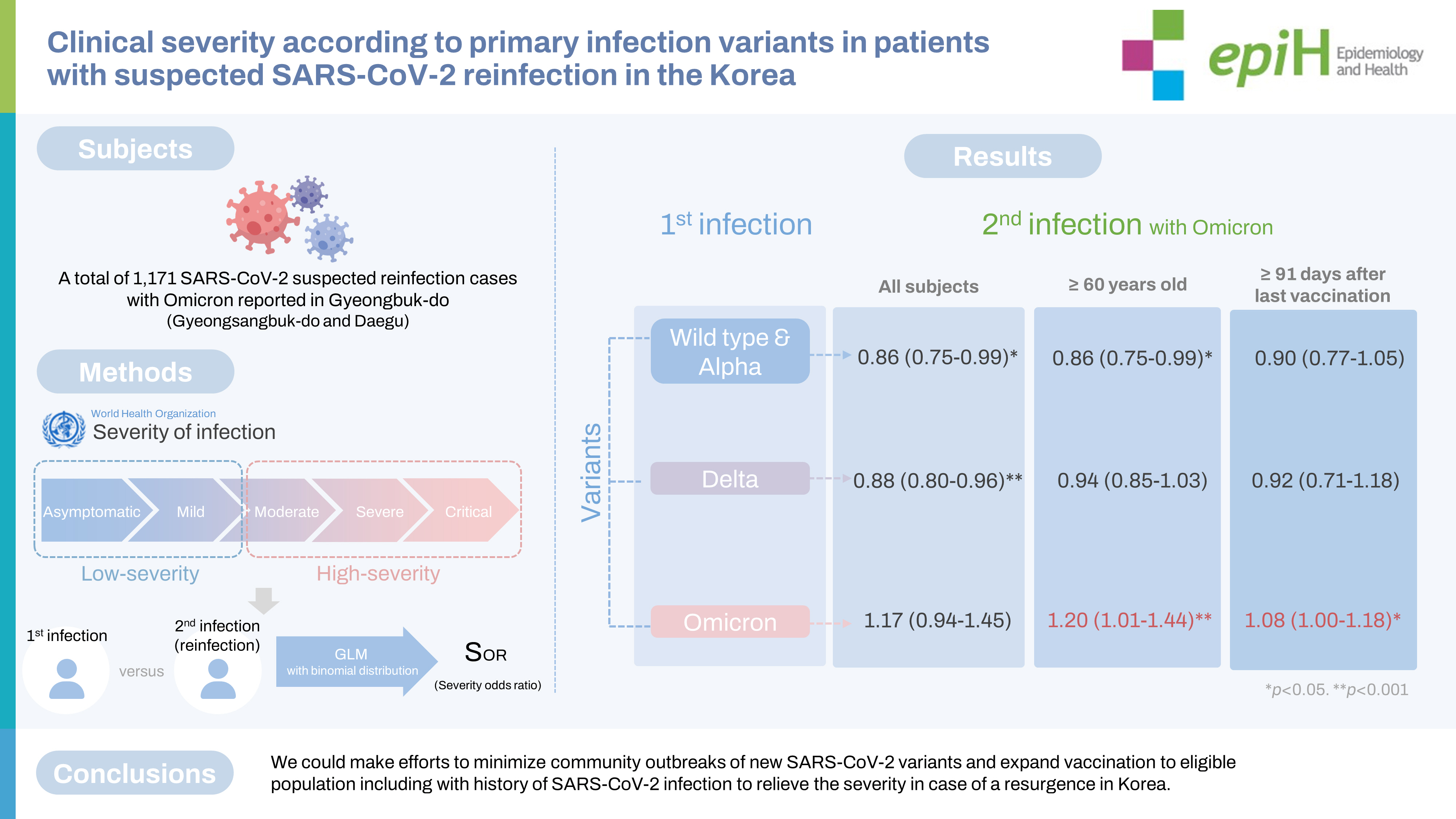
- We aimed to evaluate the severity of suspected severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) reinfection according to variants of concern in Gyeongsangbuk-do and Daegu, Korea.
-
METHODS
- The database of coronavirus disease 2019 (COVID-19) cases reported from epidemiological investigations through the integrated system operated by the Korea Disease Control and Prevention Agency, from January 20, 2020 to May 7, 2022 was combined with data from the Health Insurance Review and Assessment Service system. The severity odds ratio (SOR) in secondary infection episodes compared with primary infection was estimated using a generalized linear model with a binomial distribution.
-
RESULTS
- In all patients, the SOR of SARS-CoV-2 reinfection was 0.89 (95% confidence interval [CI], 0.82 to 0.95), and the severity was lower than in the first infection. Patients who had been vaccinated within 91 days showed a more attenuated SOR (0.85; 95% CI, 0.74 to 0.98). However, despite vaccination, in patients with both primary and secondary infections caused by the Omicron variant, the severity was reduced to a lesser extent than in patients primarily infected with other variants.
-
CONCLUSIONS
- We could make efforts to relieve the severity of COVID-19 in vulnerable populations, in which death is more likely, by recommending booster vaccinations in case of a resurgence.
- The ongoing pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is characterized by its efficient transmission [1]. Evidence from animal studies indicates that the same or different strains of SARS-CoV-2 can cause reinfection more than 21-28 days after the initial infection [2-4]. This suggests that humans are also at risk of being reinfected. According to the World Health Organization (WHO), the Alpha (B.1.1), Beta (B.1.351), Gamma (P.1), Delta (B.1.617.2), and Omicron (B.1.1.529) variants affect the retransmission, severity, diagnosis, treatment, prevention, and infection control of coronavirus disease 2019 (COVID-19) [5-8]. Previous studies have shown that, compared to other variants, Omicron poses a higher risk of reinfection [8,9]. Considering the practical effectiveness of vaccines, public concerns and questions persist regarding the severity of reinfection with new variants [8]. Moreover, the population at risk for reinfection has increased due to the possibility of COVID-19 resurgence in Korea. In this study, we aimed to estimate disease severity based on the clinical database of patients with suspected SARS-CoV-2 reinfection according to the primary variant.
INTRODUCTION
- Study subjects
- Our study was conducted using the national database of confirmed COVID-19 patients reported from epidemiological investigations through the integrated system, which is a National Notifiable Disease Surveillance System operated by the Korea Disease Control and Prevention Agency (KDCA), from January 20, 2020, to May 7, 2022 in Gyeongsangbuk-do and Daegu. According to the KDCA guidelines [10], individuals with suspected reinfection were defined as (1) those with redetected positive COVID-19 test results more than 90 days after the first infection with or without symptoms, and (2) those with redetected positive COVID-19 test results in 45-89 days after the first infection, with symptoms, exposure to a confirmed patient, or a history of overseas travel.
- During the study period, the number of patients with suspected SARS-CoV-2 reinfection was 4,297, and 4,283 patients were reinfected during the period of Omicron predominance (Table 1). Data were available on severity at the time of primary and secondary confirmation of suspected reinfection for 1,212 patients, and 1,171 patients were included to evaluate the severity of reinfection with Omicron by age group (Table 2). Among them, 824 patients received at least the first dose of COVID-19 vaccination (Table 3).
- Definition of the epidemic period
- During the study period, the KDCA conducted next-generation sequencing (NGS) analyses only if the cycle threshold value was less than 28 for samples for which a polymerase chain reaction test was obtained among epidemiologically related patients with SARS-CoV-2 infection to evaluate the timing of periods when a new variant predominated (including re-detection as a result of contact tracing). Predominance was defined as a detection rate exceeding 50.0% or more. As a result of NGS analysis, we defined the epidemic periods as involving wild-type and Alpha predominance (from January 2020 to June 2021), Delta predominance (from July to November 2021), and Omicron predominance (after December 2021) considering the diagnoses and analyses of NGS and the overall epidemic situation in Korea.
- Defining the severity of infections
- Based on the Health Insurance Review and Assessment Service system, the severity of infection was classified into 5 stages (asymptomatic, mild, moderate, severe, and critical) according to the WHO COVID-19 clinical severity scale at the time of hospital admission or treatment after confirmation [11]. We categorized the stage of asymptomatic or mild cases as low severity and moderate, severe, and critical cases as high severity in this study. The severity odds ratio (SOR) was estimated as the odds ratio for high severity versus low severity (as reference) in the secondary infection episode compared to the primary episode.
- Statistical analysis
- A generalized linear model (GLM) with a binomial distribution was used to estimate the SOR for secondary infection episodes compared to primary episodes. We calculated the SOR with adjustment for the predominant variant at the time of the primary infection, as well as sex, age, duration after the last vaccination dose, and comorbid diseases affecting the cardiovascular and endocrine systems. All statistical analyses were performed using R version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria) software, and the level of significance was set at p=0.05.
- Ethics statement
- Ethical approval was obtained from the Institutional Review Board of Sungkyunkwan University (IRB No. 2022-07-002).
MATERIALS AND METHODS
- Table 1 summarizes the demographic characteristics of the patients with suspected reinfection. In total, 4,297 patients were reinfected, and most reinfections were reconfirmed during the Omicron-predominant period. Among 4,283 patients reinfected during the Omicron dominance period, 1,933 (45.1%) of the initial infection variants were wild type and Alpha, 1,389 (32.4%) were Delta, and 961 (22.5%) were Omicron. 1,568 (36.6%) of them had never been vaccinated.
- Table 2 shows the estimated SOR of patients suspected to have SARS-CoV-2 reinfection in the Omicron-predominant period compared to the severity of the primary infection according to age group. In all patients, the SOR of reinfection was 0.89 (95% confidence interval [CI], 0.82 to 0.95), showing reduced severity compared with their first infection (SOR < 1). The severity was attenuated to a lesser extent in the second infection in patients aged ≥ 60 years (SOR, 0.89; 95% CI, 0.73 to 1.09) than in those aged < 60 years (SOR, 0.88; 95% CI, 0.80 to 0.97). However, the SOR was significantly increased in cases aged ≥ 60 years who were suspected to be infected with Omicron both primarily and reinfected (SOR, 1.20; 95% CI, 1.01 to 1.44).
- Table 3 presents the SOR of patients with suspected reinfection according to the period after their last vaccination dose. Among those vaccinated group within 91 days, vaccination significantly reduced severity. The SOR was 0.85 (95% CI, 0.74 to 0.98) and declined to a greater extent in those vaccinated within 91 days than in those for whom more than 91 days had elapsed after vaccination (SOR, 0.91; 95% CI, 0.81 to 1.03). However, despite the effect of vaccination, in patients with primary and secondary infections caused by Omicron, the level of severity of reinfection was attenuated to a lesser extent than in those who were primarily infected with other variants. In patients who had been vaccinated within 91 days, the SOR in the group primarily infected with Omicron was 1.46 times higher than that in the group primarily infected with the wild-type and Alpha variants. Furthermore, in patients for whom more than 91 days had elapsed after vaccination, the SOR significantly increased to 1.08 (95% CI, 1.00 to 1.18) among those in whom the primary and secondary infections were caused by Omicron.
RESULTS
- We observed that the severity of reinfection was alleviated in patients reinfected after primary infection with wild-type/Alpha, Delta or Omicron. The reduced severity pattern was evident even in vulnerable patients aged ≥ 60 years, but in patients with 2 episodes of Omicron infection, the severity was worsened in reinfection. When compared to the primary infection, patients with COVID-19 caused by Omicron exhibited reduced severity, especially for those who had been vaccinated within 91 days [12]. Evidence supports a large decrease in severity (comparing Omicron with Delta) and the risk of hospitalization or death [13,14]. However, these effects were weaker in patients with Omicron infection for both primary and reinfection. This suggests that the risk of reinfection is higher with the Omicron variant, which has been shown to have a marked ability to evade immunity from previous infections [9]. The severity of reinfection declined in patients in whom less than 91 days had elapsed after their last vaccination dose [15]. Based on these findings, consistent with previous studies, we suggest that vaccination provides protection, including a reduction of disease severity in the first few weeks after vaccination; however, this protection weakens over time in some individuals [16].
- Currently, we are facing a resurgence of COVID-19 infections with new recombinant variants. Therefore, we need to respond preemptively to the emergence of new variants and make efforts to implement pharmacological and non-pharmacological control strategies to protect against reinfection in elderly and vulnerable populations with low immunity due to a prolonged period after their last vaccination.
- Our study has some limitations. First, the statistical analysis was performed on severity classified into 2 values as most of the cases did not have available severity information. Therefore, it was difficult to evaluate the level of severity attenuation using the existing classification system. Second, there was a possibility of misclassifying the variants responsible for infections according to the variant predominance period. In our study, since the predominance periods were defined based on the detection rates from NGS analyses, cases of reinfection during a certain predominance period may not have actually been caused by the predominant variant. Hence, the calculated SOR may have been under-estimated or overestimated during the transitional period of variant predominance. Finally, it is also possible that the severity assessment may have been affected by the expansion of at-home treatment nationwide (from September 25, 2021) during the COVID-19 epidemic in Korea. Therefore, it is necessary to evaluate the severity with consideration of this change in the patient management system. Despite these limitations, the strength of this study lies in its evaluation of severity at the individual level of patients with suspected SARS-CoV-2 reinfection. In elderly patients with reinfection, the severity was mitigated to a lesser extent during the secondary infection episode. Vaccination was also observed to affect severity in patients with COVID-19 reinfection.
- Based on this study, we could make efforts to minimize community outbreaks of new SARS-CoV-2 variants and expand vaccination to eligible populations, including those with a history of SARS-CoV-2 infection, to attenuate the severity in case of a COVID-19 resurgence in Korea.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare for this study.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Hwang MJ, Hwang I, Park C, Park H, Kim JH. Data curation: Hwang MJ, Hwang I. Formal Analysis: Hwang MJ, Hwang I, Park C. Funding acquisition: None. Methodology: Hwang MJ, Hwang I, Kim JH. Project administration: Hwang MJ, Hwang I, Park C, Son T, Kim JH. Visualization: Hwang MJ, Hwang I, Park H, Kim JH. Writing – original draft: Hwang MJ, Kim JH. Writing – review & editing: Hwang MJ, Hwang I, Park C, Park H, Son T, Kim JH.
NOTES
ACKNOWLEDGEMENTS
| Variables |
Suspected patients with SARS-CoV-2 reinfection |
||||
|---|---|---|---|---|---|
| Wild-type and Alpha predominant | Delta predominant | Omicron predominant | p-value1 | ||
| Total | 1 (100) | 13 (100) | 4,283 (100) | 0.273 | |
| Sex | 0.463 | ||||
| Male | 0 (0.0) | 6 (46.2) | 2,005 (46.8) | ||
| Female | 1 (100) | 7 (53.8) | 2,278 (53.2) | ||
| Age (yr) | 0.925 | ||||
| 0-9 | 0 (0.0) | 1 (7.6) | 583 (13.6) | ||
| 10-19 | 0 (0.0) | 2 (15.4) | 771 (18.0) | ||
| 20-29 | 1 (100) | 4 (30.8) | 775 (18.1) | ||
| 30-39 | 0 (0.0) | 1 (7.7) | 471 (11.0) | ||
| 40-49 | 0 (0.0) | 3 (23.1) | 509 (11.9) | ||
| 50-59 | 0 (0.0) | 1 (7.7) | 422 (9.9) | ||
| 60-69 | 0 (0.0) | 1 (7.7) | 403 (9.4) | ||
| 70-79 | 0 (0.0) | 0 (0.0) | 189 (4.4) | ||
| ≥80 | 0 (0.0) | 0 (0.0) | 160 (3.7) | ||
| Underlying comorbidity2 | 0.583 | ||||
| Cardiovascular disease | 0 (0.0) | 0 (0.0) | 252 (5.9) | ||
| Respiratory diseases | 0 (0.0) | 1 (7.7) | 35 (0.8) | ||
| Endocrine diseases | 0 (0.0) | 0 (0.0) | 136 (3.2) | ||
| Digestive diseases | 0 (0.0) | 0 (0.0) | 14 (0.3) | ||
| Urinary disorders | 0 (0.0) | 0 (0.0) | 11 (0.3) | ||
| Nervous system diseases | 0 (0.0) | 0 (0.0) | 86 (2.0) | ||
| Mental disorders | 0 (0.0) | 0 (0.0) | 95 (2.2) | ||
| Neoplasms | 0 (0.0) | 0 (0.0) | 29 (0.7) | ||
| Others | 0 (0.0) | 1 (7.7) | 19 (0.4) | ||
| None | 1 (100) | 8 (61.5) | 1,938 (45.2) | ||
| Unknown | 0 (0.0) | 3 (23.1) | 1,692 (39.5) | ||
| Severity | <0.001 | ||||
| Asymptomatic | 0 (0.0) | 6 (46.1) | 114 (2.7) | ||
| Mild | 1 (100) | 5 (38.5) | 1,050 (24.5) | ||
| Moderate | 0 (0.0) | 2 (15.4) | 27 (0.6) | ||
| Severe | 0 (0.0) | 0 (0.0) | 6 (0.1) | ||
| Critical | 0 (0.0) | 0 (0.0) | 1 (0.0) | ||
| Unknown | 0 (0.0) | 0 (0.0) | 3,085 (72.0) | ||
| Vaccination | <0.05 | ||||
| Not vaccinated | 1 (100) | 13 (100) | 1,568 (36.6) | ||
| At least one dose | 0 (0.0) | 0 (0.0) | 62 (1.4) | ||
| Fully vaccinated | 0 (0.0) | 0 (0.0) | 1,266 (29.6) | ||
| First booster dose | 0 (0.0) | 0 (0.0) | 1,324 (30.9) | ||
| Second booster dose | 0 (0.0) | 0 (0.0) | 63 (1.5) | ||
| Primary infection variants | <0.05 | ||||
| Wild type and Alpha | 1 (100) | 11 (84.6) | 1,933 (45.1) | ||
| Delta | 0 (0.0) | 2 (15.4) | 1,389 (32.4) | ||
| Omicron | 0 (0.0) | 0 (0.0) | 961 (22.5) | ||
| Duration from primary infection to reinfection, mean±SD (day) | 420.0 | 274.7±194.6 | 340.0±253.3 | 0.618 | |
| Primary infection variants | All |
Age (yr) |
|
|---|---|---|---|
| <60 | ≥60 | ||
| Total | 0.89 (0.82, 0.95)*** | 0.88 (0.80, 0.97)* | 0.89 (0.73, 1.09) |
| Wild-type and Alpha | 0.86 (0.75, 0.99)* | 0.70 (0.57, 0.87)*** | 0.86 (0.75, 0.99)* |
| Delta | 0.88 (0.80, 0.96)*** | 0.89 (0.80, 0.99)* | 0.94 (0.85, 1.03) |
| Omicron | 1.17 (0.94, 1.45) | 1.11 (0.96, 1.28) | 1.20 (1.01, 1.44)*** |
Values are presented as severity odds ratio (95% confidence interval).
SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
1 The odds ratio was calculated by the severity of reinfection compared with that of the primary infection, adjusting for the variant responsible for the primary infection, sex, age, duration after the last vaccination dose, and comorbid diseases affecting the cardiovascular and endocrine systems.
* p<0.05,
*** p<0.001.
| Primary infection variants |
Duration after last vaccination dose (day) |
|
|---|---|---|
| <91 | ≥91 | |
| Total | 0.85 (0.74, 0.98)*** | 0.91 (0.81, 1.03) |
| Wild-type and Alpha | 0.61 (0.49, 0.75)*** | 0.90 (0.77, 1.05) |
| Delta | 0.86 (0.75, 0.98)*** | 0.92 (0.71, 1.18) |
| Omicron | 0.89 (0.79, 1.00) | 1.08 (1.00, 1.18)* |
Values are presented as severity odds ratio (95% confidence interval).
1 The odds ratio was calculated by the severity of reinfection compared with that of the primary infection, adjusting for the variant responsible for the primary infection, sex, age, duration after the last vaccination dose, and comorbid diseases affecting the cardiovascular and endocrine systems.
* p<0.05,
*** p<0.001.
- 1. Hu T, Liu Y, Zhao M, Zhuang Q, Xu L, He Q. A comparison of COVID-19, SARS and MERS. PeerJ 2020;8:e9725.ArticlePubMedPMCPDF
- 2. Gaudreault NN, Carossino M, Morozov I, Trujillo JD, Meekins DA, Madden DW, et al. Experimental re-infected cats do not transmit SARS-CoV-2. Emerg Microbes Infect 2021;10:638-650.ArticlePubMedPMC
- 3. Brustolin M, Rodon J, Rodríguez de la Concepción ML, Ávila-Nieto C, Cantero G, Pérez M, et al. Protection against reinfection with D614- or G614-SARS-CoV-2 isolates in golden Syrian hamster. Emerg Microbes Infect 2021;10:797-809.ArticlePubMedPMC
- 4. Deng W, Bao L, Liu J, Xiao C, Liu J, Xue J, et al. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science 2020;369:818-823.ArticlePubMed
- 5. World Health Organization. Tracking SARS-CoV-2 variants. [cited 2022 Jun 22]. Available from: https://www.who.int/activities/tracking-SARS-CoV-2-variants.
- 6. Davies NG, Abbott S, Barnard RC, Jarvis CI, Kucharski AJ, Munday JD, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science 2021;372:eabg3055.ArticlePubMedPMC
- 7. Graham MS, Sudre CH, May A, Antonelli M, Murray B, Varsavsky T, et al. Changes in symptomatology, reinfection, and transmissibility associated with the SARS-CoV-2 variant B.1.1.7: an ecological study. Lancet Public Health 2021;6:e335-e345.PubMedPMC
- 8. Ren X, Zhou J, Guo J, Hao C, Zheng M, Zhang R, et al. Reinfection in patients with COVID-19: a systematic review. Glob Health Res Policy 2022;7:12.ArticlePubMedPMCPDF
- 9. Pulliam JR, van Schalkwyk C, Govender N, von Gottberg A, Cohen C, Groome MJ, et al. Increased risk of SARS-CoV-2 reinfection associated with emergence of Omicron in South Africa. Science 2022;376:eabn4947.ArticlePubMed
- 10. Park AK, Kim IH, Rhee JE, Kim EJ, Wang SJ, Lee SE, et al. Reinfection of COVID-19 in the Republic of Korea. Public Health Wkly Rep 2021;14:2000-2004.
- 11. National Institutes of Health (NIH). COVID-19 treatment guidelines: clinical spectrum of SARS-CoV-2 infection. [cited 2022 Jun 22]. Available from: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum.
- 12. Mensah AA, Lacy J, Stowe J, Seghezzo G, Sachdeva R, Simmons R, et al. Disease severity during SARS-COV-2 reinfection: a nationwide study. J Infect 2022;84:542-550.ArticlePubMedPMC
- 13. Sigal A, Milo R, Jassat W. Estimating disease severity of Omicron and Delta SARS-CoV-2 infections. Nat Rev Immunol 2022;22:267-269.ArticlePubMedPMCPDF
- 14. Nyberg T, Ferguson NM, Nash SG, Webster HH, Flaxman S, Andrews N, et al. Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B.1.1.529) and delta (B.1.617.2) variants in England: a cohort study. Lancet 2022;399:1303-1312.ArticlePubMedPMC
- 15. Israel A, Merzon E, Schäffer AA, Shenhar Y, Green I, Golan-Cohen A, et al. Elapsed time since BNT162b2 vaccine and risk of SARS-CoV-2 infection: test negative design study. BMJ 2021;375:e067873.ArticlePubMed
- 16. Goldberg Y, Mandel M, Bar-On YM, Bodenheimer O, Freedman LS, Ash N, et al. Protection and waning of natural and hybrid immunity to SARS-CoV-2. N Engl J Med 2022;386:2201-2212.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Changes in the intrinsic severity of severe acute respiratory syndrome coronavirus 2 according to the emerging variant: a nationwide study from February 2020 to June 2022, including comparison with vaccinated populations
Boyeong Ryu, Eunjeong Shin, Dong Hwi Kim, HyunJu Lee, So Young Choi, Seong-Sun Kim, Il-Hwan Kim, Eun-Jin Kim, Sangwon Lee, Jaehyun Jeon, Donghyok Kwon, Sungil Cho
BMC Infectious Diseases.2024;[Epub] CrossRef - The effect of shortening the quarantine period and lifting the indoor mask mandate on the spread of COVID-19: a mathematical modeling approach
Jung Eun Kim, Heejin Choi, Minji Lee, Chang Hyeong Lee
Frontiers in Public Health.2023;[Epub] CrossRef - Previous infection with seasonal coronaviruses does not protect male Syrian hamsters from challenge with SARS-CoV-2
Magen E. Francis, Ethan B. Jansen, Anthony Yourkowski, Alaa Selim, Cynthia L. Swan, Brian K. MacPhee, Brittany Thivierge, Rachelle Buchanan, Kerry J. Lavender, Joseph Darbellay, Matthew B. Rogers, Jocelyne Lew, Volker Gerdts, Darryl Falzarano, Danuta M. S
Nature Communications.2023;[Epub] CrossRef

 KSE
KSE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite


