Articles
- Page Path
- HOME > Epidemiol Health > Volume 43; 2021 > Article
-
COVID-19
Systematic Review
A closer look at the high burden of psychiatric disorders among healthcare workers in Egypt during the COVID-19 pandemic -
Amr Ehab El-Qushayri1*
 , Abdullah Dahy1*
, Abdullah Dahy1* , Abdullah Reda2
, Abdullah Reda2 , Mariam Abdelmageed Mahmoud3
, Mariam Abdelmageed Mahmoud3 , Sarah Abdel Mageed3
, Sarah Abdel Mageed3 , Ahmed Mostafa Ahmed Kamel4
, Ahmed Mostafa Ahmed Kamel4 , Sherief Ghozy5
, Sherief Ghozy5
-
Epidemiol Health 2021;43:e2021045.
DOI: https://doi.org/10.4178/epih.e2021045
Published online: July 13, 2021
1Faculty of Medicine, Minia University, Minia, Egypt
2Faculty of Medicine, Al-Azhar University, Cairo, Egypt
3Faculty of Medicine, Tanta University, Tanta, Egypt
4Faculty of Pharmacy, Minia University, Minia, Egypt
5Faculty of Medicine, Mansoura University, Mansoura, Egypt
- Correspondence: Sherief Ghozy Faculty of Medicine, Mansoura University, 60 Elgomhoria Street, Mansoura 35516, Egypt E-mail: sherief_ghozy@yahoo.com
- *El-Qushayri & Dahy contributed equally to this work as joint first authors.
©2021, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
- This study aimed to examine the prevalence of psychiatric disorders among Egyptian healthcare workers (HCWs) during the coronavirus disease 2019 (COVID-19) pandemic.
-
METHODS
- Six databases were searched for relevant papers. The quality of the selected articles was measured using the National Institute of Health quality assessment tool. We used a fixed-effects model when there was no heterogeneity and a random-effects model when there was heterogeneity.
-
RESULTS
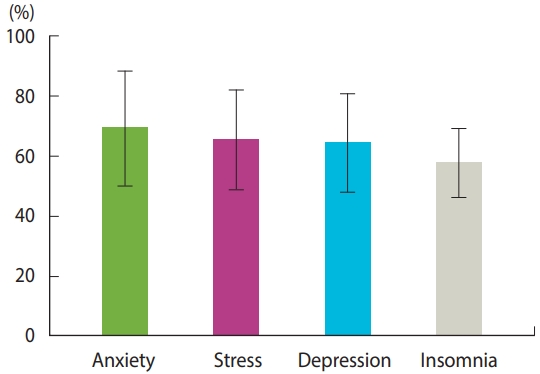
- After screening 197 records, 10 studies were ultimately included. Anxiety was the most commonly reported psychiatric disorder among HCWs, with a prevalence of 71.8% (95% confidence interval [CI], 49.4 to 86.9), followed by stress (66.6%; 95% CI, 47.6 to 81.3), depression (65.5%; 95% CI, 46.9 to 80.3), and insomnia (57.9%; 95% CI, 45.9 to 69.0). As measured using the 21-item Depression, Anxiety, and Stress Scale, the most common level of severity was moderate for depression (22.5%; 95% CI, 19.8 to 25.5) and stress (14.5%; 95% CI, 8.8 to 22.9), while high-severity anxiety was more common than other levels of severity (28.2%; 95% CI, 3.8 to 79.6).
-
CONCLUSIONS
- The COVID-19 pandemic has had a negative effect on Egyptian HCWs’ psychological well-being. More psychological support and preventive measures should be implemented to prevent the further development of psychiatric illness among physicians and other HCWs.
- Coronavirus disease 2019 (COVID-19), which emerged in Wuhan, China and is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a global pandemic by the World Health Organization (WHO) in January 2020 [1]. The basic reproductive rate for SARS-CoV-2 was estimated to be around 2.5 (ranging from 1.8 to 3.6), compared with an estimate of 2.0 to 3.0 for SARS-CoV and the influenza pandemic of 1918, 0.9 for Middle East respiratory syndrome coronavirus (MERS-CoV), and 1.5 for the influenza pandemic of 2009 [2]. Thus, SARS-CoV-2 is a highly contagious disease, especially in healthcare settings [1,3]. In Egypt, the number of cases had grown to approximately 158,000 cases and 8,696 deaths as of January 20, 2021 [4]. As a result, quarantine hospitals were designated for COVID-19 cases following a care model recommended and supervised by the WHO. Healthcare workers (HCWs) stay at different quarantine hospitals for consecutive 14-day shifts, followed by polymerase chain reaction (PCR) testing for COVID-19 infection, after which HCWs with negative tests are required to isolate in their homes for another 14 days [4]. HCWs with positive PCR results are admitted to the quarantine hospital at which they worked to receive appropriate medical care [4].
- HCWs are the first line of defense during any health crisis, including for past outbreaks of Ebola, scarlet fever, measles, H1N1, H5N1, MERS, and SARS, with the COVID-19 pandemic being the most recent health crisis [5]. During the COVID-19 pandemic, as in previous outbreaks, personal protection is quickly exhausted, workloads are increased, and fears about infection or infection of family members pose a psychological burden on HCWs [6]. Severe anxiety, depression, insomnia, and stress have all been reported by Egyptian HCWs who have treated COVID-19 patients [6,7]. These conditions have a significant effect on HCWs’ work performance, decision-making, and concentration [5], which can lead to work-related diseases and injuries [8]. Moreover, occupational stress has been found to affect HCWs’ intentions to leave work and their professions in the long term [9]. A combination of possible exposure and stress also increases HCWs’ susceptibility to COVID-19 infection [10]. Thus, this study aimed to examine the prevalence of psychiatric disorders among Egyptian HCWs during the COVID-19 outbreak through a systematic review and meta-analysis.
INTRODUCTION
- Search strategy and study selection
- On December 30, 2020 (updated on January 15, 2021), a systematic search of 6 databases was performed following the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines [11]. The 6 databases were Google Scholar, Scopus, the System for Information on Grey Literature in Europe, PubMed, the New York Academy of Medicine, and Web of Science, and the search keywords were (COVID-19 OR COVID 19 OR novel coronavirus) AND (mental health OR depression OR anxiety OR insomnia OR psychology) AND (Egypt). A manual search was conducted after the systematic search to include all relevant papers that may have been missed by the systematic search.
- All papers on the prevalence of psychiatric disorders among Egyptian HCWs during the COVID-19 outbreak were included. Studies that examined non-HCWs or non-Egyptians, multicenter studies from which data on Egyptian HCWs could not be extracted, review papers, and conference abstracts were all excluded.
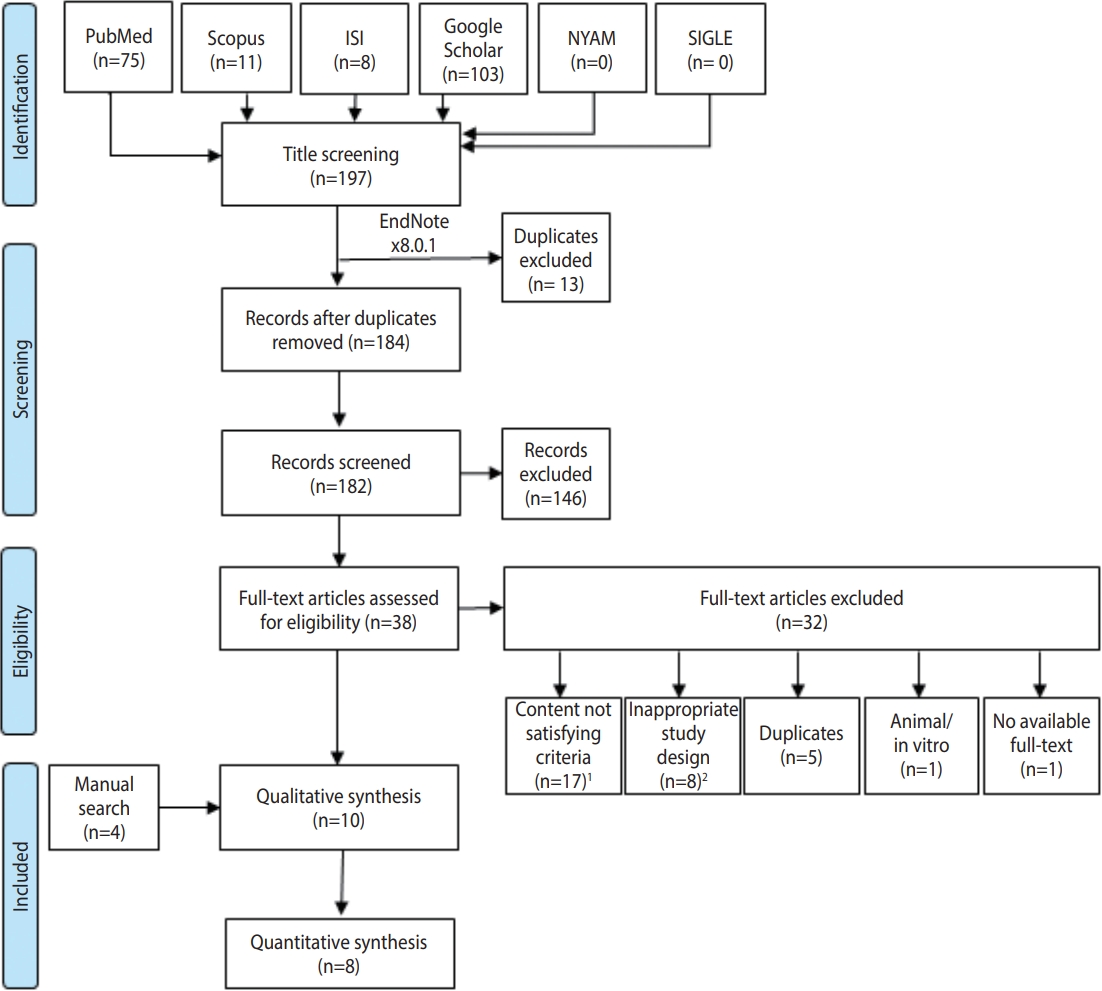
- Following the systematic search, duplicate articles were excluded using EndNote version X8 (Thompson Reuters, Carlsbad, CA, USA). Title and abstract screening was initially performed by 2 authors (AEE and AD), and full-text screening was performed by 5 authors (AEE, AR, MAM, SAM, and AMAK). A senior author (SG) was appointed to resolve any conflicts and identify errors.
- Data extraction
- A senior author (AEE) developed an extraction template that consisted of 3 parts. The first part was for study characteristics (reference ID, study design, age of participants, sample size, the percentage of male HCWs, the percentage of HCWs who worked in quarantine hospitals, the specific roles of the HCWs, and the scale used for measuring psychiatric disorders). The second part was for the prevalence and severity of psychiatric disorders, and the last part was for the quality rating of each study.
- Risk of bias
- All of the included studies were cross-sectional; therefore, the National Institute of Health quality assessment tool was used [12]. We classified the quality of each study into the following 3 categories: 1 for good quality (10-14 points), 2 for fair quality (5-9 points), and 3 for poor quality (0-4 points).
- Statistical analysis
- Comprehensive Meta-Analysis version 3 (Biostat Inc., Englewood, NJ, USA) was used to analyze the collected data. We calculated the event rate and its corresponding 95% confidence intervals (CIs) for different psychiatric disorders. Subgroup analysis was conducted based on scores from the 21-item Depression, Anxiety, and Stress Scale (DASS-21), which is the most commonly used scale for measuring psychiatric disorders. Subgroup analysis was not performed when the subgroup consisted of 3 or fewer studies. We used a random-effects model if heterogeneity was found among the pooled results measured using an I2 value of > 50% or a p-value of < 0.05 [13]. Otherwise, a fixed-effects model was used. If any outcome was reported in 10 or more studies, a meta-regression or Egger regression (publication bias) analysis was performed [14,15]. Publication bias was considered significant for p-values of < 0.1 in the Egger test.
- Ethics statement
- Ethical approval was not applicable as this is a secondary analysis of published papers.
MATERIALS AND METHODS
- Search results and study characteristics
- In total, 197 records were discovered during the online database search. Of these, 13 were considered duplicates and were excluded before the title and abstract screening. Out of the remaining 184 records, 38 papers were eligible for full-text screening, after which 6 studies were included. Four additional papers were found via a manual search. In total, 10 studies from the database search were included in the analysis (Figure 1 and Table 1) (Supplementary Material 1).
- All 10 studies were cross-sectional and had a cumulative sample size of 3,137 HCWs. Six studies included only physicians as participants, 2 included only nurses, one included physicians and nurses, and one included physicians, nurses, pharmacists, house officers, technicians, and others (Table 1).
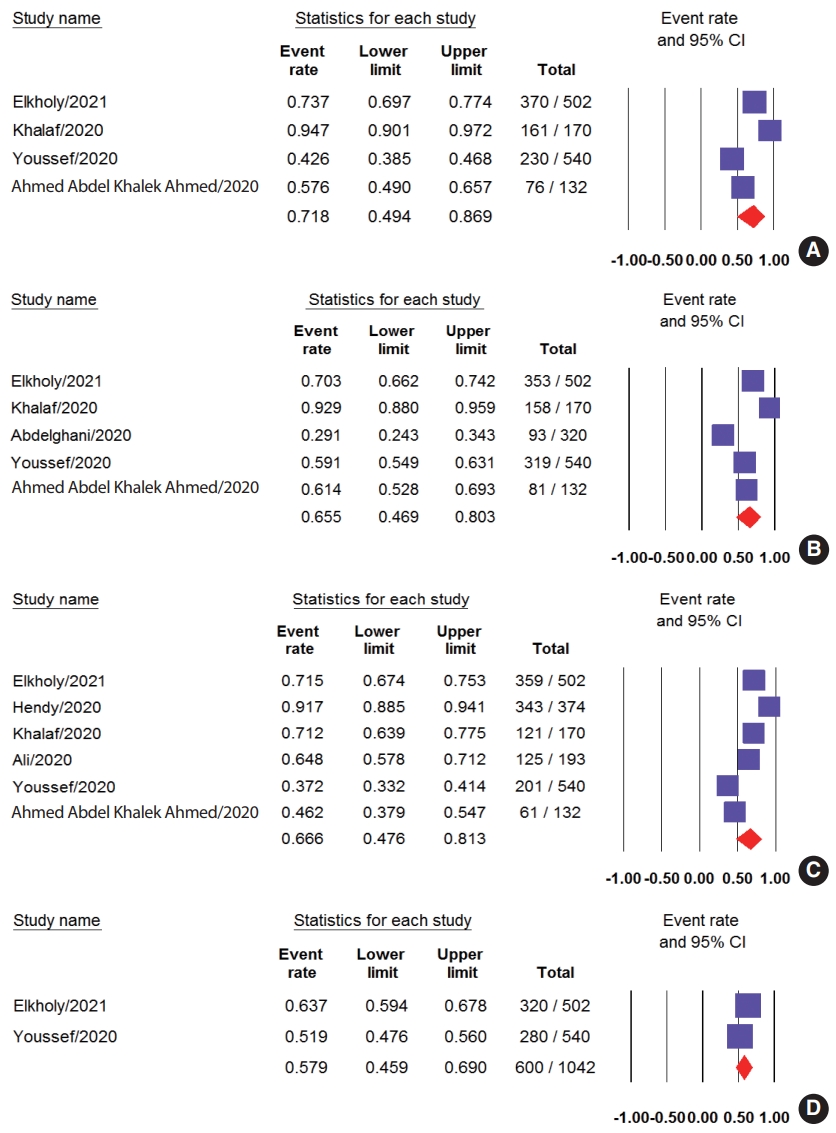
- Anxiety
- Of the 4 studies that assessed anxiety among HCWs, 3 used the DASS-21 [4,16,17], and one used the Patient Health Questionnaire (PHQ) [6]. The overall prevalence of anxiety was high, at 71.8% (95% CI, 49.4 to 86.9), with 28.2% (95% CI, 3.8 to 79.6) of the participants reporting severe forms of anxiety (Figures 2 and 3A). Moderate, mild, and severe anxiety had prevalence rates of 12.3% (95% CI, 6.1 to 23.1), 9.9% (95% CI, 4.9 to 19.0), and 6.4% (95% CI, 4.9 to 8.3), respectively (Supplementarty Materials 2-5). A random-effects model was adopted for all analyses due to significant heterogeneity (p < 0.001) except for severe anxiety, for which there was no heterogeneity (p= 0.42).
- Depression
- Five studies examined the prevalence of depression among HCWs, with 3 of them using the DASS-21 scale [4,16,17], 1 using the PHQ [6], and 1 using the Hospital Anxiety and Depression Scale [18]. The pooled depression prevalence was 65.5% (95% CI, 46.9 to 80.3); however, the results showed significant heterogeneity (p< 0.001, I2 = 98%) (Figures 2 and 3B). Moderate depression was the most common type of depression in terms of severity, with a prevalence of 22.5% (95% CI, 19.8 to 25.5), followed by very severe depression (16.3%; 95% CI, 5.4 to 39.9), severe depression (16.1%; 95% CI, 8.3 to 28.9), and mild depression (12.5%; 95% CI, 8.0 to 19.0) (Supplementary Materials 6-9). Nevertheless, significant heterogeneity was found for severe and mild depression (p< 0.001), while moderate depression showed no heterogeneity (p= 0.42).
- Stress
- Seven studies examined stress experienced by HCWs. Three studies used the DASS-21 [4,16,17], 2 studies used the Perceived Stress Scale [6,19], and 2 used the Nursing Stress Scale [7,20]. The pooled prevalence of stress was 66.6% (95% CI, 47.6 to 81.3) (Figures 2 and 3C). Moderate stress was the most common type of stress experienced by HCWs (14.5%; 95% CI, 8.8 to 22.9) followed by severe, mild, and very severe stress, with rates of 14.3% (95% CI, 10.0 to 20.1), 11.5% (95% CI, 9.5 to 13.9), and 9.3% (95% CI, 3.2 to 24.0), respectively (Supplementary Materials 10-13). We used a random-effects model to analyze the total prevalence and severity of anxiety due to the presence of significant heterogeneity (p< 0.001) except for moderate severity, for which significant heterogeneity was not found.
- Insomnia
- Insomnia was examined in 2 studies, both of which measured insomnia using the Insomnia Severity Index [4,6]. The rate of insomnia among HCWs was 57.9% (95% CI, 45.9 to 69.0) (Figures 2 and 3D).
- Burnout
- One study measured the prevalence of burnout among 220 physicians using the Maslach Burnout Inventory Human Services Survey [21]. The prevalence of burnout was 36%.
- Distress
- One study examined the prevalence of distress among 266 HCWs, which was measured using the Peritraumatic Distress Index [22]. The total prevalence of distress was 67%. Of those with distress, 52% experienced mild and moderate distress and 15% experienced severe distress.
- Death ideation
- Only one study examined death ideation among HCWs. Across a total of 320 physicians, 35 physicians reported having death ideation, with a prevalence of 11% [18].
RESULTS
- Under normal circumstances, the risk of HCWs developing a psychiatric disorder is higher than that of workers in other occupations and the general population [23,24]. During the COVID-19 pandemic, the risk is even higher as HCWs are required to make major psychological and physical efforts to face the burden caused by the pandemic. Such burdens can have a major impact on the quality of care provided to patients due to an increase in medical errors, which in turn further increase the burden on healthcare systems [25-27].
- In the present study, we aimed to gather further evidence on the prevalence of psychiatric disorders among Egyptian HCWs to draw attention to their experiences, provide support to address their struggles, and improve the quality of provided care. Our analysis showed that the prevalence of reported psychological symptoms was notably high, as previously mentioned. The rates of psychological illness found in this study were much higher than those found in studies about HCWs in other countries, including China [28] and Italy [29]. In Singapore and India, a similar multinational study was conducted and found that the prevalence rates for anxiety, depression, and stress were 15.7%, 10.6%, and 5.2%, respectively, which are much lower than the estimated prevalence rates found in the present study [30]. Another meta-analysis found that the prevalence rates of anxiety and depression were 23.2% and 22.8%, respectively [31]. A more recent meta-analysis also found similar prevalence rates of psychiatric illnesses among HCWs, with estimated prevalence rates of 24.3%, 25.8%, and 45.0% for depression, anxiety, and stress, respectively [32]. Comparing these numbers to our results clearly shows the degree to which the Egyptian healthcare system was burdened by the COVID-19 pandemic and indicates an urgent need for effective solutions to reduce the burden.
- The prevalence of psychiatric symptoms was higher among HCWs in Egypt during the COVID-19 pandemic than in the preCOVID-19 era. A cross-sectional study conducted at Alexandria University that recruited nurses in critical care units found prevalence rates of 51%, 69%, and 50% for depression, anxiety, and stress, respectively, among nurses [33]. In addition, Al-Sayed et al. [34] conducted a cross-sectional study on residents at Ain Shams University that found that 53% of residents were affected with mild to moderate depression. After the start of the COVID-19 pandemic, and according to our results, there has been a noticeable rise in psychiatric symptoms experienced by HCWs, including anxiety (71.8%), stress (66.6%), depression (65.5%), and insomnia (57.9%).
- Many reasons can be attributed to the high estimated prevalence of psychological disorders among HCWs. First, the effects of the pandemic and the negative emotions related to the millions of people who were infected and subsequent hundreds of thousands of deaths. Such feelings are heightened for HCWs, who are in direct contact with COVID-19 patients [10,35]. Such feelings are possibly even worse among HCWs who work in areas other than infectious diseases since they may lack experience and not know how to deal appropriately with respiratory illnesses or use personal protective equipment [36]. In addition, Egyptian HCWs are subject to intensive workloads, including potential 24-hour shifts, to compensate for the shortage of HCWs in the Egyptian healthcare system. This, combined with shortages in medical supplies and low wages received by Egyptian HCWs, are potential risk factors for developing psychological disorders. Moral distress is another possible explanation for the decrease in the mental health of HCWs since they are forced to work only with the resources available to them [35,37]. Lack of direct support for HCWs from supervisors and a heightened culture of blame for potential mistakes is also a potential factor that influences the prevalence of psychiatric disorders among HCWs [7]. Additionally, HCWs may be exposed to unexplained stress and even violence from patients and their families due to the decreased quality of care [8]. Social stigmatization is also a factor that influences HCWs’ mental health since people may have safety concerns about interacting with HCWs who are in direct contact with COVID-19 patients [38].
- Our findings indicate an urgent need for proper interventions to increase the quality of care in Egyptian healthcare facilities. The Egyptian Ministry of Health already provides a direct hotline for HCWs to report their needs and make urgent requests. Further measures should also be urgently undertaken to decrease the high prevalence rate of psychological disorders among HCWs. We suggest that HCWs should be vaccinated as efficiently as possible and receive adequate personal protective equipment to reduce their risk of COVID-19 infection [39]. Improving the quality of life of HCWs might also relieve HCWs’ psychological symptoms and encourage them to keep working in Egypt’s healthcare system [40-42]. Organizing the daily shifts of HCWs and better distributing their work hours are also recommended; however, this should be done based on available resources [43].
- Our results are limited to the small number of studies included in our analysis and the small sample size of the included studies. Moreover, heterogeneity in our results may be a result of differences in proportion of male HCWs, the role of HCWs, and the scales used to measure psychiatric illnesses in the included studies.
DISCUSSION
- The COVID-19 pandemic has had an unfavorable effect on the psychological well-being of Egyptian HCWs. More psychological support and preventive measure should be implemented to prevent HCWs from developing major psychiatric illnesses. Collaborative efforts between policymakers, hospital executives, members of the media, and the general population are urgently needed to address this issue.
CONCLUSION
SUPPLEMENTARY MATERIALS
Supplementary Material 1.
Supplementary Material 2.
Supplementary Material 3.
Supplementary Material 4.
Supplementary Material 5.
Supplementary Material 6.
Supplementary Material 7.
Supplementary Material 8.
Supplementary Material 9.
Supplementary Material 10.
Supplementary Material 11.
Supplementary Material 12.
Supplementary Material 13.
-
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare for this study.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: AEE. Data curation: AEE, AD, AR, MAM, SAM, AMAK. Formal analysis: AEE. Funding acquisition: None. Methodology: AEE, AD, SG. Project administration: AEE, SG. Writing – original draft: AEE, AD, AR, MAM, SAM, AMAK. Writing – review & editing: SG.
NOTES
ACKNOWLEDGEMENTS
| Study | Study design | Works in quarantine hospital, n (%) | Sample size | Age (mean ±SD or range), yr | Sex, male | Type of health care workers (%) | Risk of bias |
|---|---|---|---|---|---|---|---|
| Elkholy et al., 2021 [6] | Cross-sectional | 237 (47.2) | 502 | >18 | 251 | Physicians (60.0), nurses (40.0) | Fair |
| Abdelhafiz et al., 2020 [21] | Cross-sectional | NR | 220 | 33.42±5.3 | 111 | Physicians (100) | Fair |
| Hendy et al., 2020 [20] | Cross-sectional | 374 (100) | 374 | 32.06±3.9 | 122 | Nurses (100) | Fair |
| Khalaf et al., 2020 [16] | Cross-sectional | NR | 170 | 36.47±5.1 | 66 | Physicians (100) | Fair |
| Abdelghani et al., 2020 [18] | Cross-sectional | NR | 320 | 34.6±6.0 | 117 | Physicians (100) | Fair |
| Said et al., 2021 [7] | Cross-sectional | 210 (50.0) | 420 | 20-59 | 76 | Nurses (100) | Fair |
| Ali et al., 2020 [19] | Cross-sectional | NR | 193 | NR | NR | Physicians (100) | Fair |
| Youssef et al., 2020 [4] | Cross-sectional | 55 (10.2) | 540 | 37.3±9.2 | 294 | Physicians (77.0), nurses (9.0), pharmacists (7.0), house officer (2.0), Technician (2.0), other (3.0) | Fair |
| Abasiri et al., 2020 [22] | Cross-sectional | NR | 266 | NR | NR | NR | Fair |
| Ahmed Abdel Khalek Ahmed et al., 2020 [17] | Cross-sectional | NR | 132 | 24.6 | 3.3 | Nurses (100) | Fair |
- 1. World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19); 2020 [cited 2021 Mar 1]. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.PDF.
- 2. Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis 2020;20:e238-e244.ArticlePubMedPMC
- 3. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199-1207.ArticlePubMedPMC
- 4. Youssef N, Mostafa A, Ezzat R, Yosef M, El Kassas M. Mental health status of health-care professionals working in quarantine and nonquarantine Egyptian hospitals during the COVID-19 pandemic. East Mediterr Health J 2020;26:1155-1164.ArticlePubMed
- 5. Jun J, Tucker S, Melnyk BM. Clinician mental health and wellbeing during global healthcare crises: evidence learned from prior epidemics for COVID-19 pandemic. Worldviews Evid Based Nurs 2020;17:182-184.ArticlePubMed
- 6. Elkholy H, Tawfik F, Ibrahim I, Salah El-Din W, Sabry M, Mohammed S, et al. Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: a call for action. Int J Soc Psychiatry 2021;67:522-531.ArticlePubMed
- 7. Said RM, El-Shafei DA. Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ Sci Pollut Res Int 2021;28:8791-8801.ArticlePubMed
- 8. Hassan NM, Abu-Elenin MM, Elsallamy RM, Kabbash IA. Job stress among resident physicians in Tanta University Hospitals, Egypt. Environ Sci Pollut Res Int 2020;27:37557-37564.ArticlePubMed
- 9. Lo WY, Chien LY, Hwang FM, Huang N, Chiou ST. From job stress to intention to leave among hospital nurses: a structural equation modelling approach. J Adv Nurs 2018;74:677-688.ArticlePubMed
- 10. Neto MLR, Almeida HG, Esmeraldo JD, Nobre CB, Pinheiro WR, de Oliveira CR, et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res 2020;288:112972.ArticlePubMedPMC
- 11. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100.ArticlePubMedPMC
- 12. National Heart, Lung, and Blood Institute (NIH). Quality assessment tool for observational cohort and cross-sectional studies. [cited 2021 Mar 1]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 13. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions: version 5.1.0; 2011 [cited 2021 Mar 1]. Available from: https://handbook-5-1.cochrane.org/.
- 14. Egger M, Davey Smith G, Schneider M, Minder C. Bias in metaanalysis detected by a simple, graphical test. BMJ 1997;315:629-634.ArticlePubMedPMC
- 15. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA 2006;295:676-680.ArticlePubMed
- 16. Khalaf OO, Khalil MA, Abdelmaksoud R. Coping with depression and anxiety in Egyptian physicians during COVID-19 pandemic. Middle East Curr Psychiatry 2020;27:1-7.Article
- 17. Ahmed Abdel Khalek Ahmed H, Mohamed Metwaly Atia S. Psychological problems and fear of COVID-19 pandemic among nurses and general population: a comparative Study. Egypt J Health Care 2020;11:500-524.Article
- 18. Abdelghani M, El-Gohary HM, Fouad E, Hassan MS. Addressing the relationship between perceived fear of COVID-19 virus infection and emergence of burnout symptoms in a sample of Egyptian physicians during COVID-19 pandemic: a cross-sectional study. Middle East Curr Psychiatry 2020;27:1-9.Article
- 19. Ali H, Ismail AA, Abdalwahab A. Mental stress in anesthesia and intensive care physicians during COVID-19 outbreak. Anesth Pain Med 2020;10:e106623.ArticlePubMedPMC
- 20. Hendy A, Abozeid A, Sallam G, Abboud Abdel Fattah H, Ahmed Abdelkader Reshia F. Predictive factors affecting stress among nurses providing care at COVID-19 isolation hospitals at Egypt. Nurs Open 2020;8:498-505.ArticlePubMedPMC
- 21. Abdelhafiz AS, Ali A, Ziady HH, Maaly AM, Alorabi M, Sultan EA. Prevalence, associated factors, and consequences of burnout among Egyptian physicians during COVID-19 pandemic. Front Public Health 2020;8:590190.ArticlePubMedPMC
- 22. Abasiri RA, RilleraMarzo R, Abdelaziz H, Abdelaziz H. Evaluating the psychological distress of the coronavirus disease 2019 pandemic in Egypt. Eur J Mol Clin Med 2020;7:1-12.
- 23. Kim MS, Kim T, Lee D, Yook JH, Hong YC, Lee SY, et al. Mental disorders among workers in the healthcare industry: 2014 national health insurance data. Ann Occup Environ Med 2018;30:31.ArticlePubMedPMC
- 24. Suzuki K, Ohida T, Kaneita Y, Yokoyama E, Miyake T, Harano S, et al. Mental health status, shift work, and occupational accidents among hospital nurses in Japan. J Occup Health 2004;46:448-454.ArticlePubMed
- 25. Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surg 2010;251:995-1000.ArticlePubMed
- 26. Crijns TJ, Kortlever JT, Guitton TG, Ring D, Barron GC. Symptoms of burnout among surgeons are correlated with a higher incidence of perceived medical errors. HSS J 2020;16(Suppl 2):305-310.ArticlePubMedPMC
- 27. Trockel MT, Menon NK, Rowe SG, Stewart MT, Smith R, Lu M, et al. Assessment of physician sleep and wellness, burnout, and clinically significant medical errors. JAMA Netw Open 2020;3:e2028111.ArticlePubMed
- 28. Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr 2020;33:e100259.ArticlePubMedPMC
- 29. Lasalvia A, Bonetto C, Porru S, Carta A, Tardivo S, Bovo C, et al. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiol Psychiatr Sci 2020;30:e1.ArticlePubMed
- 30. Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun 2020;88:559-565.ArticlePubMedPMC
- 31. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020;88:901-907.ArticlePubMedPMC
- 32. Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health 2020;18:100.ArticlePubMedPMC
- 33. Abd El-aal NH, Hassan NI. Relationships between staff nurses’ satisfaction with quality of work and their levels of depression, anxiety, and stress in critical care units. J Am Sci 2014;10:91-101.
- 34. Al-Sayed NN, Elsheikh MM, Mahmoud DA, El-Ghamry RH, Sabry WM, et al. Work stress: psychological impact and correlates in a sample of Egyptian medical residents. Middle East Curr Psychiatry 2016;23:113-118.
- 35. Oh N, Hong N, Ryu DH, Bae SG, Kam S, Kim KY. Exploring nursing intention, stress, and professionalism in response to infectious disease emergencies: the experience of local public hospital nurses during the 2015 MERS outbreak in South Korea. Asian Nurs Res (Korean Soc Nurs Sci) 2017;11:230-236.ArticlePubMedPMC
- 36. Wu Y, Wang J, Luo C, Hu S, Lin X, Anderson AE, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage 2020;60:e60-e65.ArticlePubMedPMC
- 37. Simonds AK, Sokol DK. Lives on the line? Ethics and practicalities of duty of care in pandemics and disasters. Eur Respir J 2009;34:303-309.ArticlePubMed
- 38. Fischer LS, Mansergh G, Lynch J, Santibanez S. Addressing disease-related stigma during infectious disease outbreaks. Disaster Med Public Health Prep 2019;13:989-994.ArticlePubMedPMC
- 39. Centers for Disease Control Prevention. COVID-19 vaccines for healthcare personnel. 2020 Dec 28 [cited 2021 Jan 18]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/hcp.html.
- 40. Farid S, El-Deen AN, El-Batrawy R. Egypt Household International Migration Survey 2013: main findings and key indicators. Cairo: Central Agency for Public Mobilization and Statistics; 2015. p 1-6.
- 41. Jenkins R, Kydd R, Mullen P, Thomson K, Sculley J, Kuper S, et al. International migration of doctors, and its impact on availability of psychiatrists in low and middle income countries. PLoS One 2010;5:e9049.ArticlePubMedPMC
- 42. Loza N, Sorour E. Brain drain: the issues raised for Egypt by the emigration of psychiatrists. BJPsych Int 2016;13:59-61.ArticlePubMedPMC
- 43. Riklikienė O, Krušinskaitė D, Gatautis R, Bagdonaitė Ž. Nurses’ work-related stress, job satisfaction, and intent to leave: a survey in primary health care centers. NERP 2015;5:11-20.
REFERENCES
Figure & Data
References
Citations

- Stress, anxiety, depression and sleep disturbance among healthcare professional during the COVID-19 pandemic: An umbrella review of 72 meta-analyses
Mohammed Al Maqbali, Ahmad Alsayed, Ciara Hughes, Eileen Hacker, Geoffrey L. Dickens, Fadwa Alhalaiqa
PLOS ONE.2024; 19(5): e0302597. CrossRef - Anxiety and stress among healthcare professionals during COVID-19 in Ethiopia: systematic review and meta-analysis
Aragaw Asfaw Hasen, Abubeker Alebachew Seid, Ahmed Adem Mohammed
BMJ Open.2023; 13(2): e070367. CrossRef - COVID-19 and common mental health symptoms in the early phase of the pandemic: An umbrella review of the evidence
Anke B. Witteveen, Susanne Y. Young, Pim Cuijpers, José Luis Ayuso-Mateos, Corrado Barbui, Federico Bertolini, Maria Cabello, Camilla Cadorin, Naomi Downes, Daniele Franzoi, Michael Gasior, Brandon Gray, Maria Melchior, Mark van Ommeren, Christina Palantz
PLOS Medicine.2023; 20(4): e1004206. CrossRef - Effectiveness of mindfulness-based interventions on burnout and self-compassion among critical care nurses caring for patients with COVID-19: a quasi-experimental study
Sahar Younes Othman, Nagia I. Hassan, Alaa Mostafa Mohamed
BMC Nursing.2023;[Epub] CrossRef - COVID‐19 outcomes in paediatric cancer: A large scale pooled meta‐analysis of 984 cancer patients
Amr Ehab El‐Qushayri, Amira Yasmine Benmelouka, Abdullah Dahy, Mohammad Rashidul Hashan
Reviews in Medical Virology.2022;[Epub] CrossRef - Mental health symptoms during the COVID-19 pandemic in developing countries: A systematic review and meta-analysis
Jiyao Chen, Stephen X Zhang, Allen Yin, Jaime A Yáñez
Journal of Global Health.2022;[Epub] CrossRef - Scientific evidence on mental health in key regions under the COVID-19 pandemic – meta-analytical evidence from Africa, Asia, China, Eastern Europe, Latin America, South Asia, Southeast Asia, and Spain
Stephen X. Zhang, Jiyao Chen
European Journal of Psychotraumatology.2021;[Epub] CrossRef

 KSE
KSE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite




